Exhibit 99.2

Transformative immunomodulating medicines for patients January 2025 1
2 Forward Looking Statements This presentation contains “forward-looking
statements” within the meaning of the safe harbor provisions of the Private Securities Litigation Reform Act of 1995. Words such as “may”, “will”, “believe”, “expect”, “plan”, “anticipate”, “estimate” and similar expressions (as well as
other words or expressions referencing future events or circumstances) are intended to identify forward-looking statements. All statements, other than statements of historical facts, included in this presentation are forward-looking
statements. These statements include, but are not limited to, Immunocore’s capabilities across oncology, autoimmune and infectious disease therapeutic areas and its ability to grow, and further development the PRAME portfolio; the estimated
market size and patient population for KIMMTRAK and Immunocore’s other product candidates; the three growth areas of KIMMTRAK, including HLA-A02+ melanoma, cutaneous melanoma and adjuvant uveal melanoma; expected submission of
investigational new drug applications or clinical trial applications; the potential regulatory approval, expected clinical benefits and availability of Immunocore’s product candidates; the commercial performance of KIMMTRAK including
indication expansion; the potential benefits and advantages KIMMTRAK, brenetafusp and Immunocore’s other product candidates will provide for patients; the potential of the PRAME portfolio opportunity to expand into additional solid tumor
indications; expectations regarding the design, progress, timing, enrollment, scope, expansion, funding, and results of Immunocore’s existing and planned clinical trials, those of Immunocore’s collaboration partners or the combined clinical
trials with Immunocore’s collaboration partners; the timing and sufficiency of clinical trial outcomes to support potential approval of any of Immunocore’s product candidates or those of, or combined with, its collaboration partners;
expected commercial and clinical milestones and Immunocore’s ability to achieve those milestones on their expected timeline, or at all; the value of Immunocore’s products and product candidates for patients and shareholders; and potential
growth opportunities and trends, including in connection with product launches. Any forward-looking statements are based on management’s current expectations and beliefs of future events and are subject to a number of risks and
uncertainties that could cause actual events or results to differ materially and adversely from those set forth in or implied by such forward-looking statements, many of which are beyond Immunocore’s control. These risks and uncertainties
include, but are not limited to, the impact of worsening macroeconomic conditions on Immunocore’s business, financial position, strategy and anticipated milestones, including Immunocore’s ability to conduct ongoing and planned clinical
trials; Immunocore’s ability to obtain a clinical supply of current or future product candidates or commercial supply of KIMMTRAK or any future approved products, including as a result of health epidemics or pandemics, war in Ukraine, the
conflict in the Middle East, the broader risk of a regional conflict in the Middle East, or global geopolitical tension; Immunocore’s ability to obtain and maintain regulatory approval of its product candidates, including KIMMTRAK;
Immunocore’s ability and plans in continuing to establish and expand a commercial infrastructure and to successfully launch, market and sell KIMMTRAK and any future approved products; Immunocore’s ability to successfully expand the approved
indications for KIMMTRAK or obtain marketing approval for KIMMTRAK in additional geographies in the future; the delay of any current or planned clinical trials, whether due to patient enrollment delays or otherwise; Immunocore’s ability to
successfully demonstrate the safety and efficacy of its product candidates and gain approval of its product candidates on a timely basis, if at all; competition with respect to market opportunities; unexpected safety or efficacy data
observed during preclinical studies or clinical trials; actions of regulatory agencies, which may affect the initiation, timing and progress of clinical trials or future regulatory approval; Immunocore’s need for and ability to obtain
additional funding, on favorable terms or at all, including as a result of worsening macroeconomic conditions, including changes inflation and interest rates and unfavorable general market conditions, and the impacts thereon of the war in
Ukraine, the conflict in the Middle East, and global geopolitical tension; Immunocore’s ability to obtain, maintain and enforce intellectual property protection for KIMMTRAK or any product candidates it or its collaborators are developing;
and the success of Immunocore’s current and future collaborations, partnerships or licensing arrangements, including the risk that Immunocore may not realize the anticipated benefits of its collaboration with Bristol Myers Squibb. These and
other risks and uncertainties are described in greater detail in the section titled "Risk Factors" in Immunocore’s filings with the Securities and Exchange Commission, including Immunocore’s most recent Annual Report on Form 10-K for the
year ended December 31, 2023 filed with the Securities and Exchange Commission on February 28, 2024, as well as discussions of potential risks, uncertainties, and other important factors in Immunocore’s subsequent filings with the
Securities and Exchange Commission. All forward looking statements contained in this presentation speak only as of the date on which they were made and should not be relied upon as representing its views as of any subsequent date. Except
to the extent required by law, Immunocore undertakes no obligation to update such statements to reflect events that occur or circumstances that exist after the date on which they were made. Certain information contained in this
presentation relates to or is based on studies, publications, surveys, and other data obtained from third party sources and Immunocore’s own internal estimates and research. While Immunocore believes these third party sources to be reliable
as of the date of this presentation, it has not independently verified, and makes no representation as to the adequacy, fairness, accuracy, or completeness of, any information obtained from third party sources. KIMMTRAK is a trademark
owned or licensed to Immunocore.
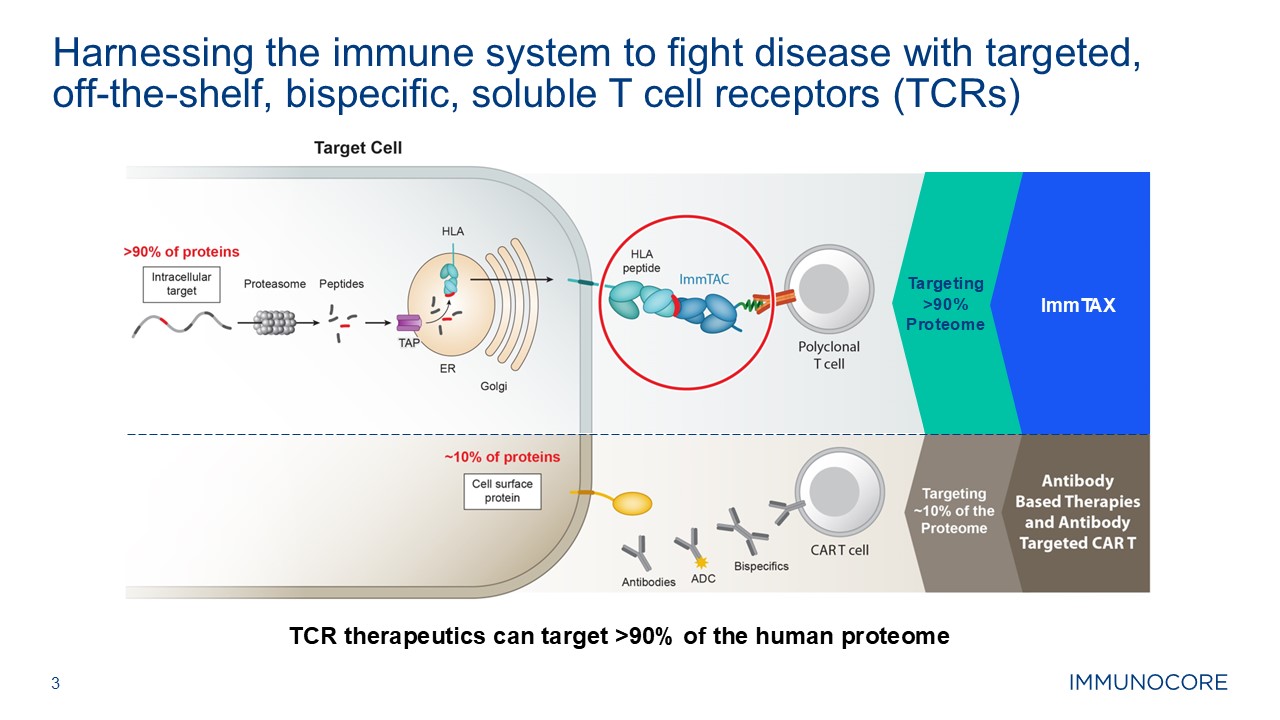
3 Harnessing the immune system to fight disease with targeted, off-the-shelf,
bispecific, soluble T cell receptors (TCRs) TCR therapeutics can target >90% of the human proteome ImmTAX Targeting >90% Proteome
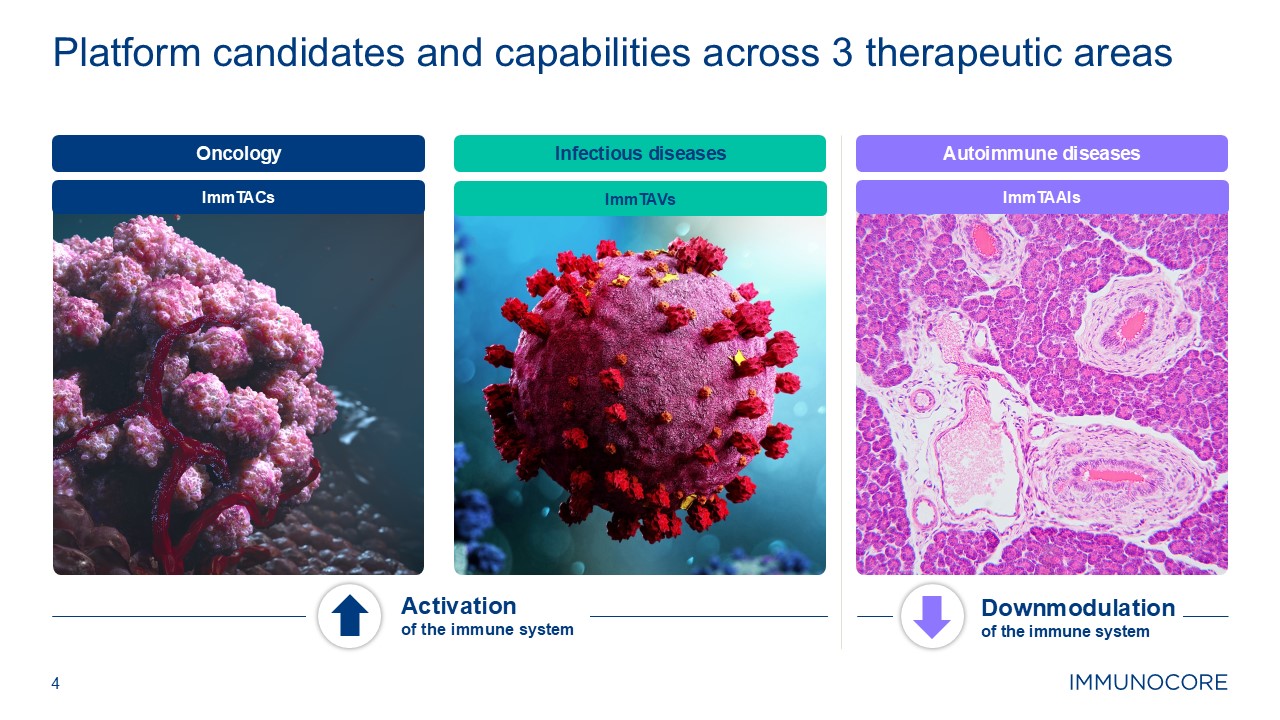
4 Platform candidates and capabilities across 3 therapeutic areas Activation
of the immune system Downmodulation of the immune system Infectious diseases Autoimmune diseases ImmTACs ImmTAVs ImmTAAIs Oncology
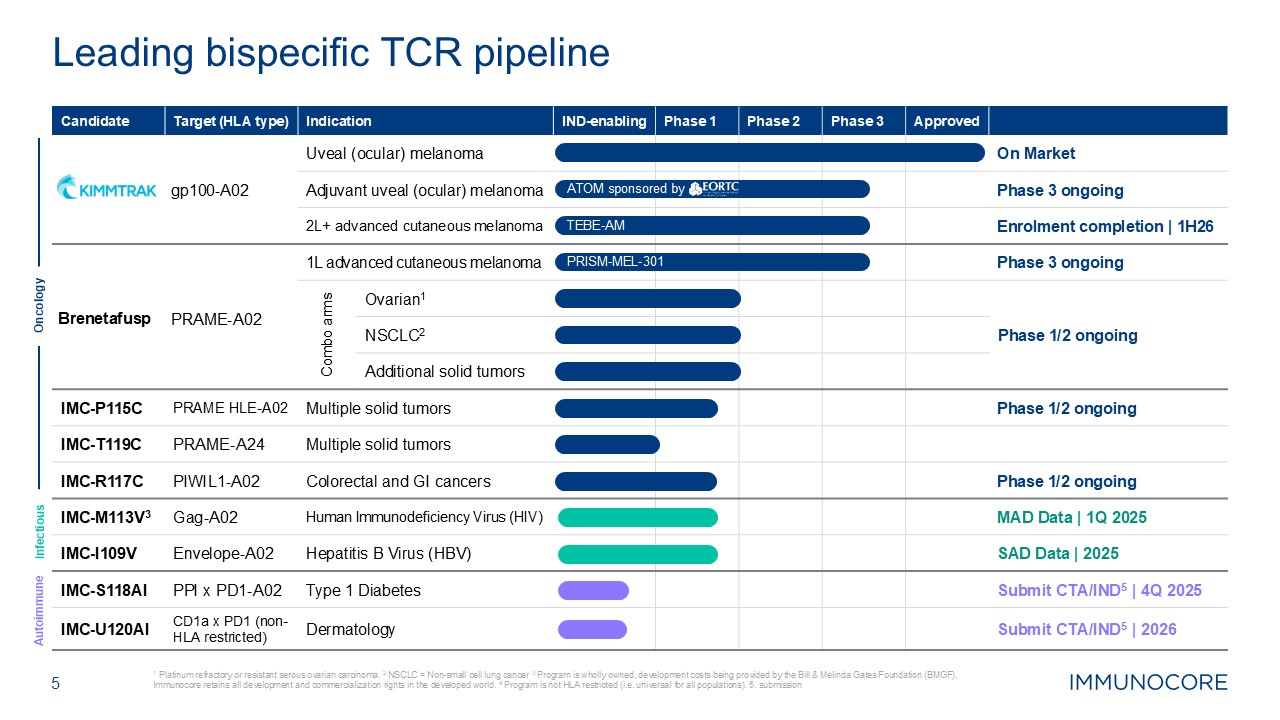
5 1 Platinum refractory or resistant serous ovarian carcinoma. 2 NSCLC =
Non-small cell lung cancer 3 Program is wholly owned, development costs being provided by the Bill & Melinda Gates Foundation (BMGF), Immunocore retains all development and commercialization rights in the developed world. 4 Program is
not HLA restricted (i.e. universal for all populations). 5. submission Leading bispecific TCR pipeline Candidate Target (HLA type) Indication IND-enabling Phase 1 Phase 2 Phase 3 Approved gp100-A02 Uveal (ocular) melanoma On
Market Adjuvant uveal (ocular) melanoma Phase 3 ongoing 2L+ advanced cutaneous melanoma Enrolment completion | 1H26 Brenetafusp PRAME-A02 1L advanced cutaneous melanoma Phase 3 ongoing Combo arms Ovarian1 Phase 1/2
ongoing NSCLC2 Additional solid tumors IMC-P115C PRAME HLE-A02 Multiple solid tumors Phase 1/2 ongoing IMC-T119C PRAME-A24 Multiple solid tumors IMC-R117C PIWIL1-A02 Colorectal and GI cancers Phase 1/2
ongoing IMC-M113V3 Gag-A02 Human Immunodeficiency Virus (HIV) MAD Data | 1Q 2025 IMC-I109V Envelope-A02 Hepatitis B Virus (HBV) SAD Data | 2025 IMC-S118AI PPI x PD1-A02 Type 1 Diabetes Submit CTA/IND5 | 4Q 2025 IMC-U120AI CD1a
x PD1 (non-HLA restricted) Dermatology Submit CTA/IND5 | 2026 Oncology Infectious Autoimmune TEBE-AM PRISM-MEL-301 ATOM sponsored by
Maximizing potential of KIMMTRAK® in HLA‑A02+ melanoma 6
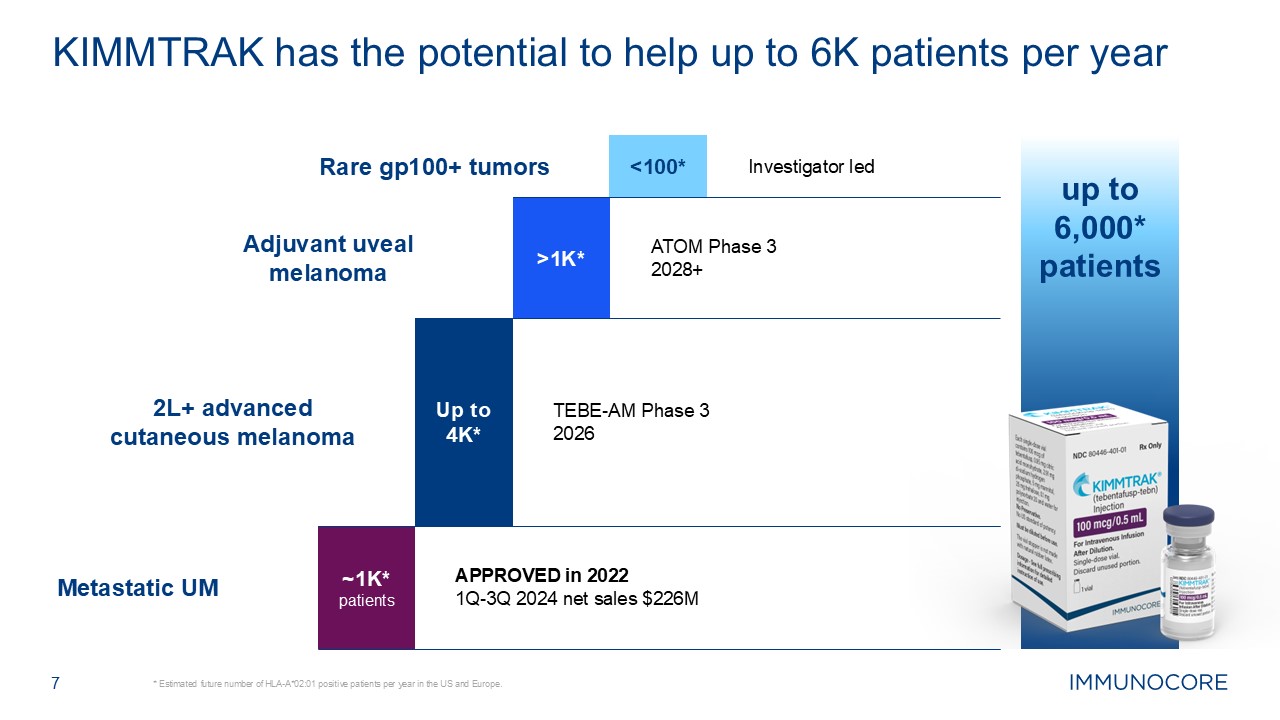
up to 6,000* patients 7 * Estimated future number of HLA-A*02:01 positive
patients per year in the US and Europe. KIMMTRAK has the potential to help up to 6K patients per year ~1K* patients Up to 4K* >1K* 2L+ advanced cutaneous melanoma <100* APPROVED in 2022 1Q-3Q 2024 net sales $226M TEBE-AM
Phase 3 2026 ATOM Phase 3 2028+ Investigator led Adjuvant uveal melanoma Rare gp100+ tumors Metastatic UM
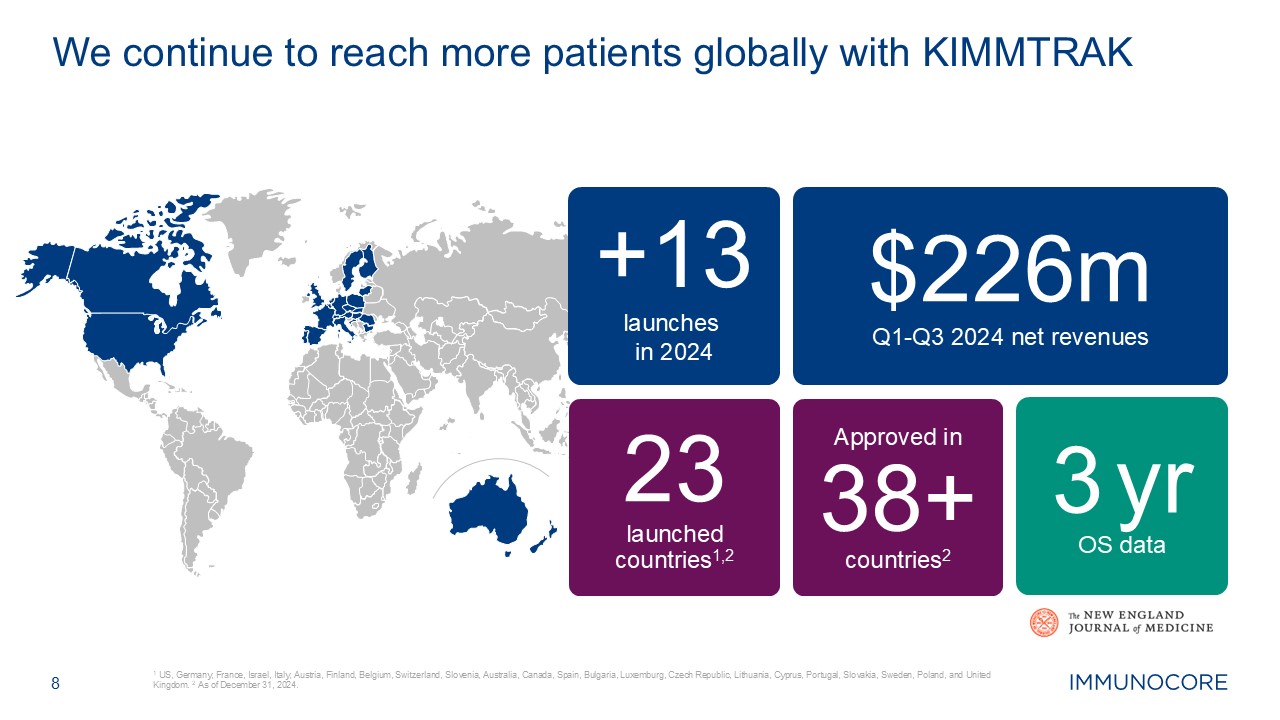
8 1 US, Germany, France, Israel, Italy, Austria, Finland, Belgium,
Switzerland, Slovenia, Australia, Canada, Spain, Bulgaria, Luxemburg, Czech Republic, Lithuania, Cyprus, Portugal, Slovakia, Sweden, Poland, and United Kingdom. 2 As of December 31, 2024. We continue to reach more patients globally with
KIMMTRAK $226m Q1-Q3 2024 net revenues +13 launches in 2024 Approved in 38+ countries2 23 launchedcountries1,2 3 yr OS data
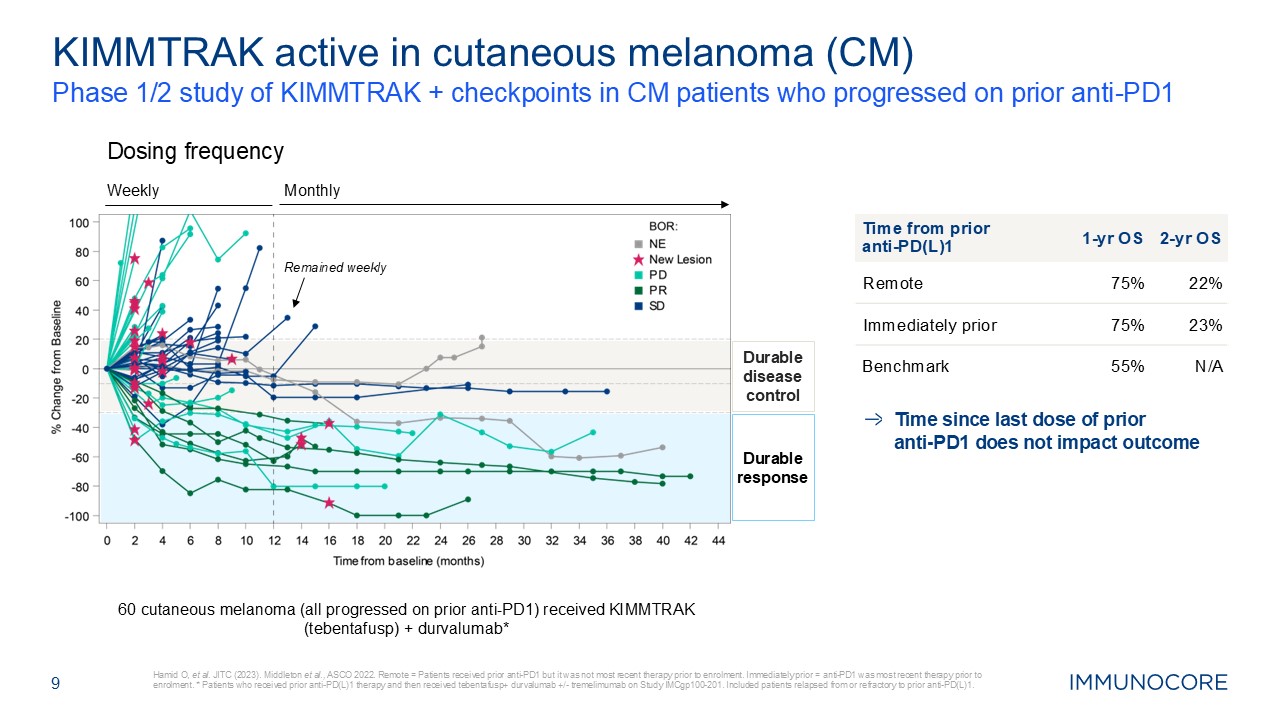
9 Phase 1/2 study of KIMMTRAK + checkpoints in CM patients who progressed on
prior anti-PD1 Hamid O, et al. JITC (2023). Middleton et al., ASCO 2022. Remote = Patients received prior anti-PD1 but it was not most recent therapy prior to enrolment. Immediately prior = anti-PD1 was most recent therapy prior to
enrolment. * Patients who received prior anti-PD(L)1 therapy and then received tebentafusp+ durvalumab +/- tremelimumab on Study IMCgp100-201. Included patients relapsed from or refractory to prior anti-PD(L)1. KIMMTRAK active in cutaneous
melanoma (CM) Time from prior anti‑PD(L)1 1-yr OS 2-yr OS Remote 75% 22% Immediately prior 75% 23% Benchmark 55% N/A Weekly Monthly Dosing frequency Remained weekly Durable response Durable disease control 60
cutaneous melanoma (all progressed on prior anti-PD1) received KIMMTRAK (tebentafusp) + durvalumab* Time since last dose of prior anti‑PD1 does not impact outcome
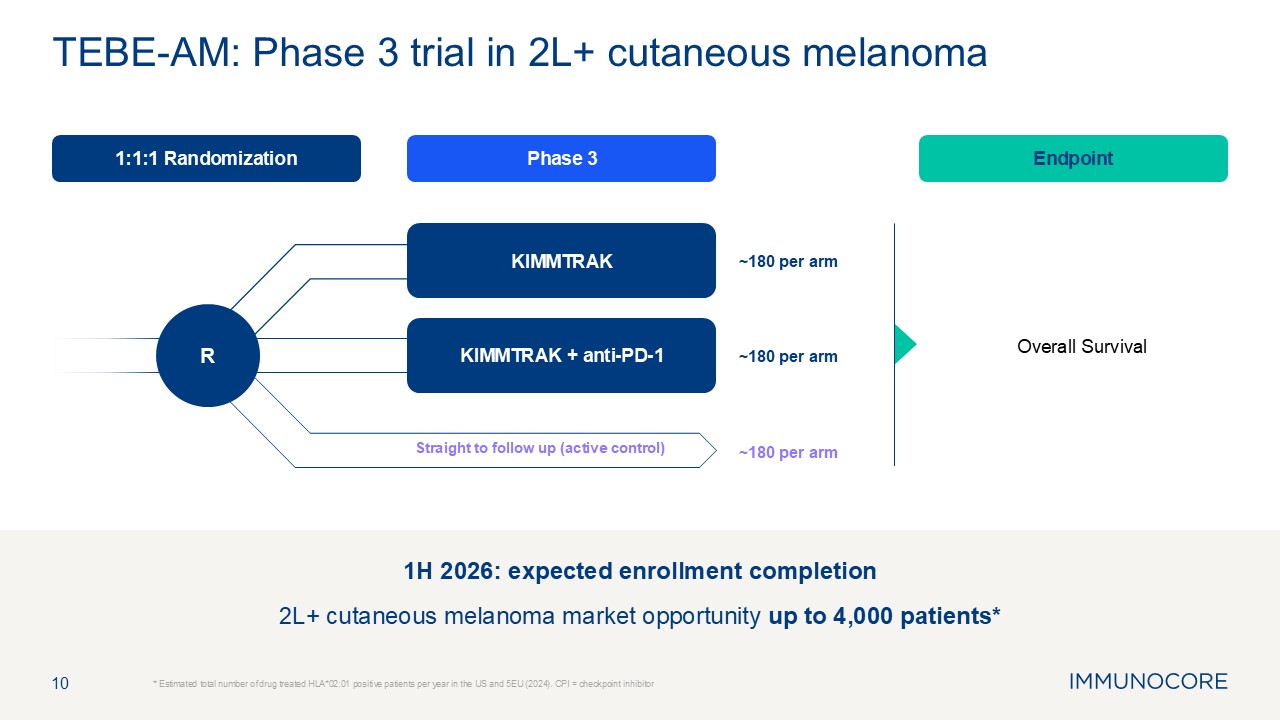
10 * Estimated total number of drug treated HLA*02:01 positive patients
per year in the US and 5EU (2024). CPI = checkpoint inhibitor TEBE-AM: Phase 3 trial in 2L+ cutaneous melanoma Phase 3 Endpoint 1:1:1 Randomization Overall Survival KIMMTRAK KIMMTRAK + anti-PD-1 Straight to follow up (active
control) R ~180 per arm ~180 per arm ~180 per arm 1H 2026: expected enrollment completion 2L+ cutaneous melanoma market opportunity up to 4,000 patients*
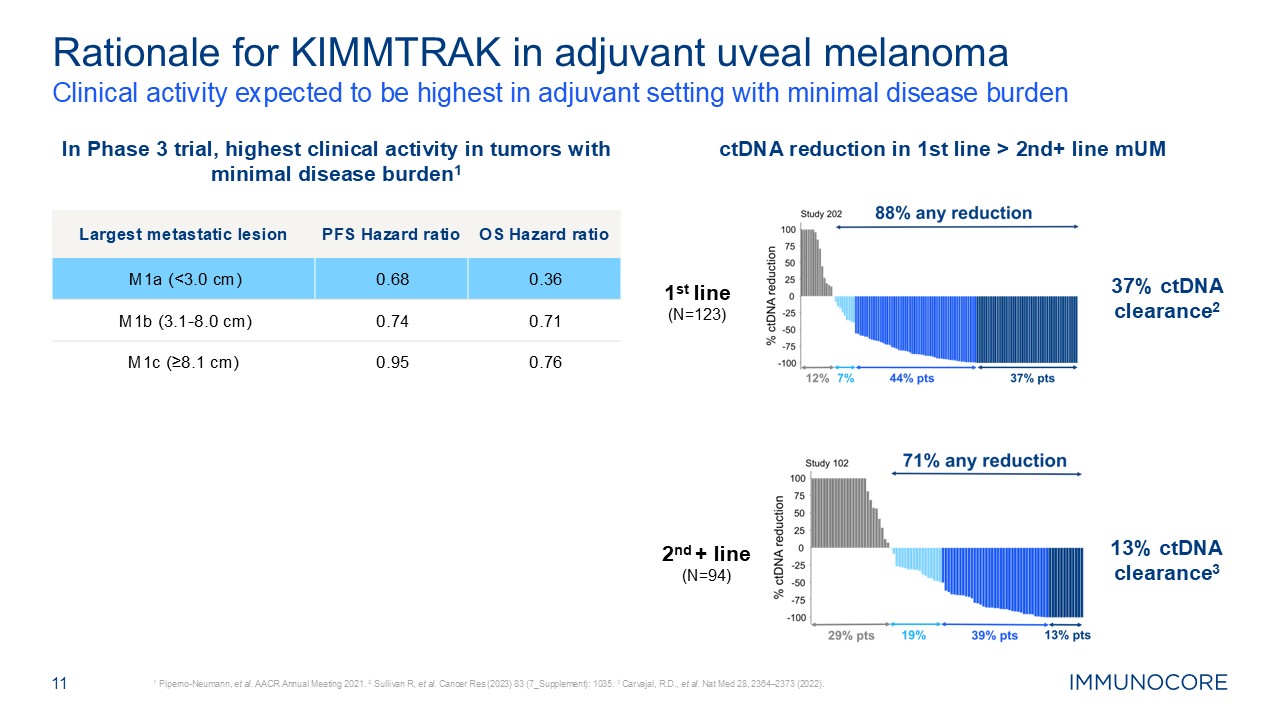
Clinical activity expected to be highest in adjuvant setting with minimal
disease burden 1 Piperno-Neumann, et al. AACR Annual Meeting 2021. 2 Sullivan R, et al. Cancer Res (2023) 83 (7_Supplement): 1035. 3 Carvajal, R.D., et al. Nat Med 28, 2364–2373 (2022). 11 Rationale for KIMMTRAK in adjuvant uveal
melanoma In Phase 3 trial, highest clinical activity in tumors with minimal disease burden1 ctDNA reduction in 1st line > 2nd+ line mUM 1st line (N=123) 37% ctDNA clearance2 2nd + line (N=94) 13% ctDNA clearance3 Largest
metastatic lesion PFS Hazard ratio OS Hazard ratio M1a (<3.0 cm) 0.68 0.36 M1b (3.1-8.0 cm) 0.74 0.71 M1c (≥8.1 cm) 0.95 0.76
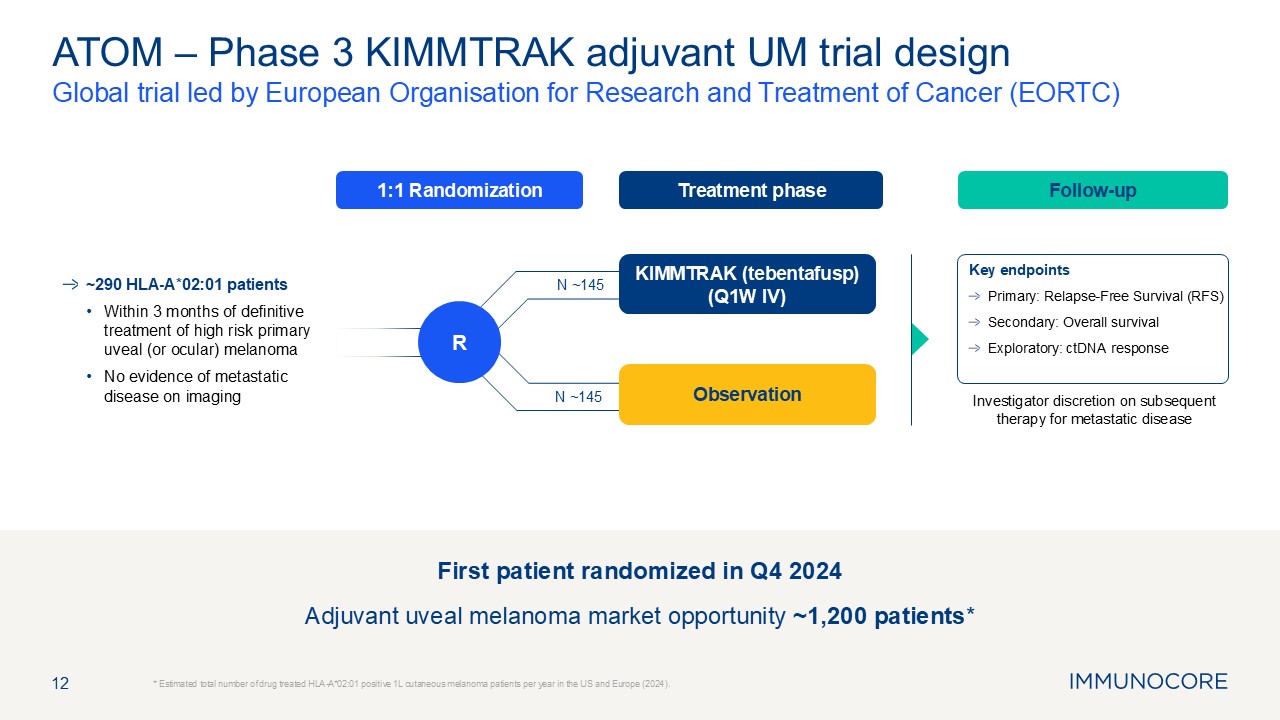
Treatment phase Follow-up 1:1 Randomization 12 Global trial led by
European Organisation for Research and Treatment of Cancer (EORTC) * Estimated total number of drug treated HLA-A*02:01 positive 1L cutaneous melanoma patients per year in the US and Europe (2024). ATOM – Phase 3 KIMMTRAK adjuvant UM
trial design Investigator discretion on subsequent therapy for metastatic disease KIMMTRAK (tebentafusp) (Q1W IV) R ~290 HLA-A*02:01 patients Within 3 months of definitive treatment of high risk primary uveal (or ocular) melanoma No
evidence of metastatic disease on imaging Key endpoints Primary: Relapse-Free Survival (RFS) Secondary: Overall survival Exploratory: ctDNA response Observation First patient randomized in Q4 2024 Adjuvant uveal melanoma market
opportunity ~1,200 patients* N ~145 N ~145

PRAME portfolio 13
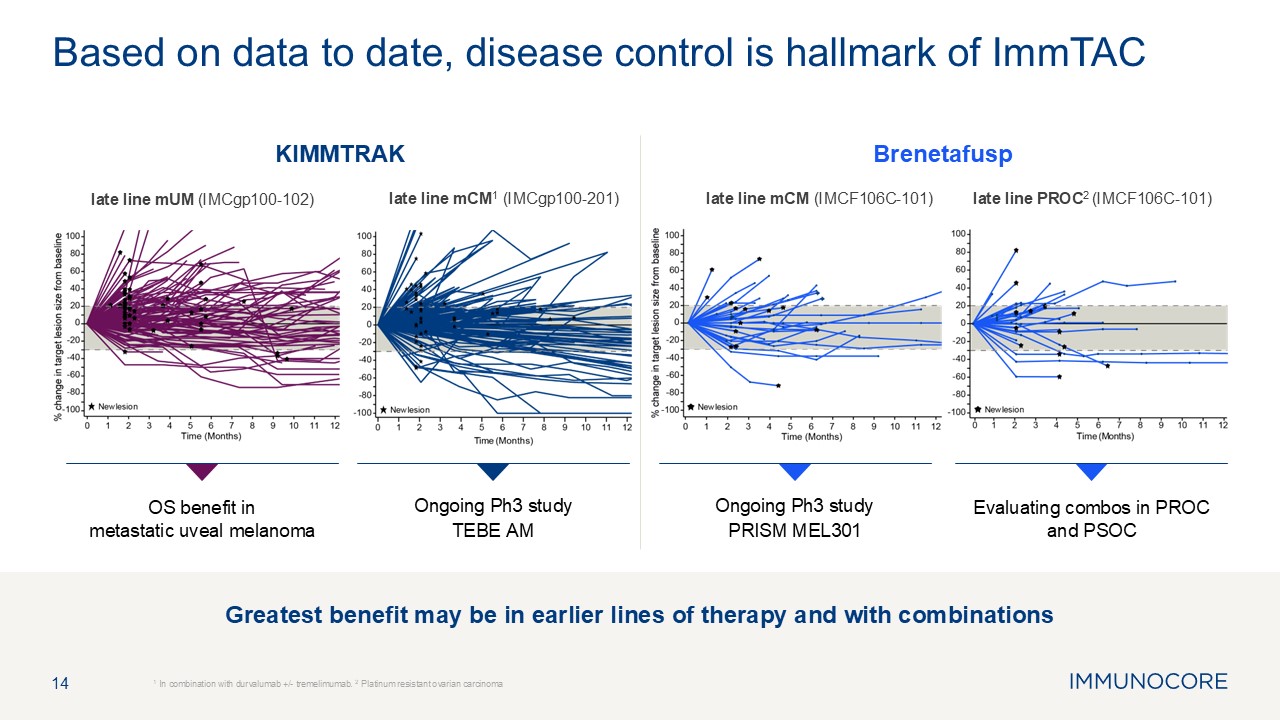
Greatest benefit may be in earlier lines of therapy and with
combinations 14 1 In combination with durvalumab +/- tremelimumab. 2 Platinum resistant ovarian carcinoma Based on data to date, disease control is hallmark of ImmTAC Ongoing Ph3 study PRISM MEL301 Evaluating combos in PROC and
PSOC Brenetafusp late line mUM (IMCgp100-102) OS benefit inmetastatic uveal melanoma Ongoing Ph3 study TEBE AM KIMMTRAK late line mCM1 (IMCgp100-201) late line mCM (IMCF106C-101) late line PROC2 (IMCF106C-101)
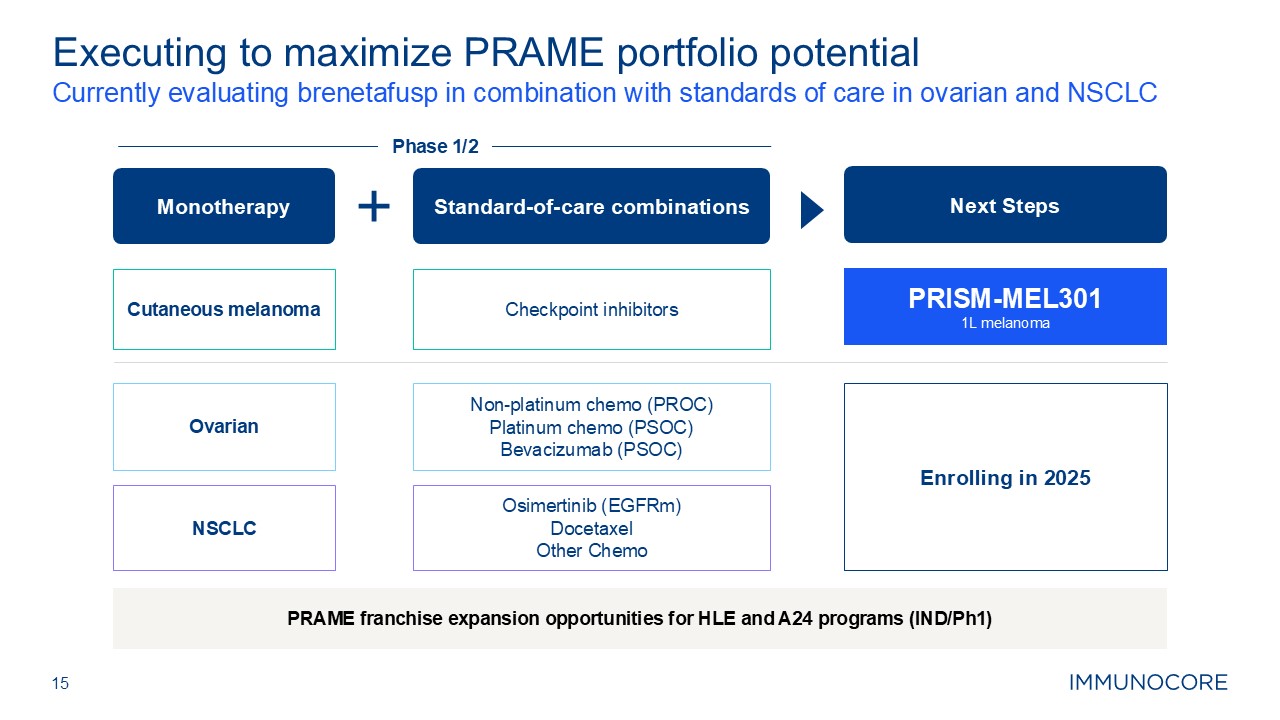
15 Currently evaluating brenetafusp in combination with standards of care in
ovarian and NSCLC Executing to maximize PRAME portfolio potential Monotherapy Standard-of-care combinations Checkpoint inhibitors NSCLC Ovarian Cutaneous melanoma Next Steps PRISM-MEL301 1L melanoma Non-platinum chemo
(PROC) Platinum chemo (PSOC) Bevacizumab (PSOC) Osimertinib (EGFRm) Docetaxel Other Chemo Enrolling in 2025 Phase 1/2 PRAME franchise expansion opportunities for HLE and A24 programs (IND/Ph1)

Brenetafusp in cutaneous melanoma 16
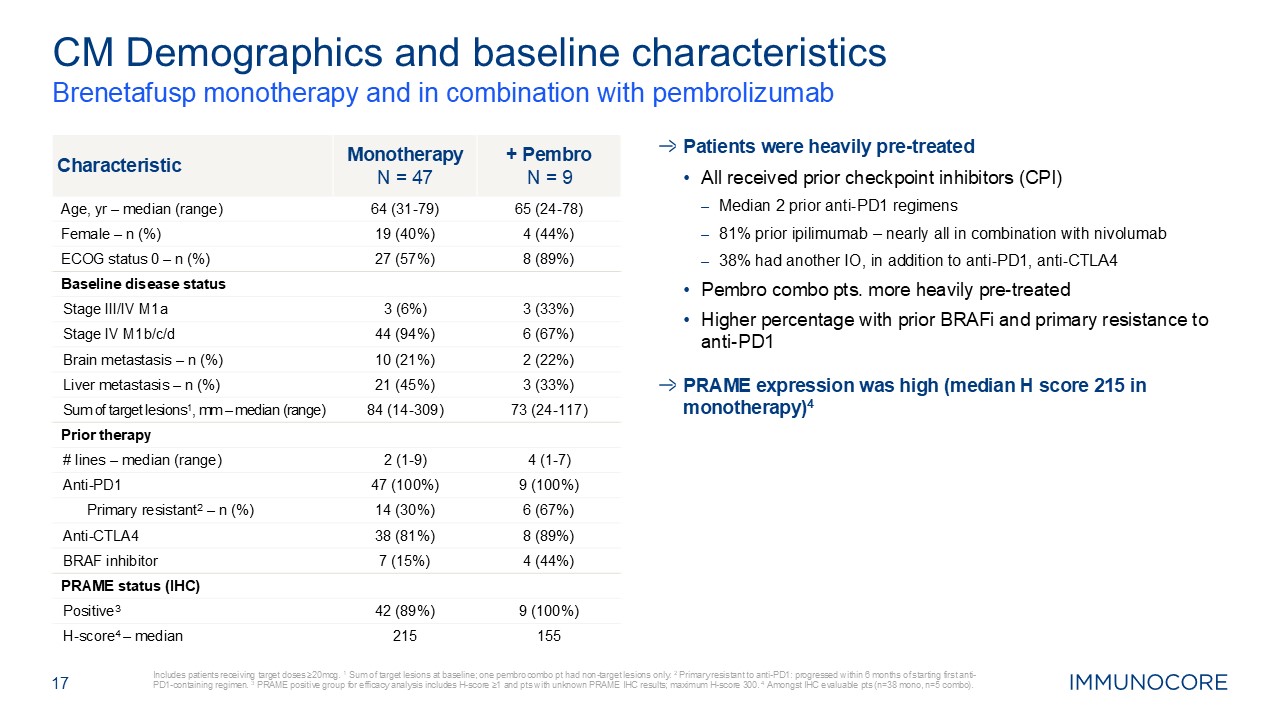
Brenetafusp monotherapy and in combination with pembrolizumab Includes
patients receiving target doses ≥20mcg. 1 Sum of target lesions at baseline; one pembro combo pt had non-target lesions only. 2 Primary resistant to anti-PD1: progressed within 6 months of starting first anti-PD1-containing regimen. 3 PRAME
positive group for efficacy analysis includes H-score ≥1 and pts with unknown PRAME IHC results; maximum H-score 300. 4 Amongst IHC evaluable pts (n=38 mono, n=5 combo). 17 CM Demographics and baseline
characteristics Characteristic Monotherapy N = 47 + Pembro N = 9 Age, yr – median (range) 64 (31-79) 65 (24-78) Female – n (%) 19 (40%) 4 (44%) ECOG status 0 – n (%) 27 (57%) 8 (89%) Baseline disease status Stage III/IV
M1a 3 (6%) 3 (33%) Stage IV M1b/c/d 44 (94%) 6 (67%) Brain metastasis – n (%) 10 (21%) 2 (22%) Liver metastasis – n (%) 21 (45%) 3 (33%) Sum of target lesions1, mm – median (range) 84 (14-309) 73 (24-117) Prior therapy #
lines – median (range) 2 (1-9) 4 (1-7) Anti-PD1 47 (100%) 9 (100%) Primary resistant2 – n (%) 14 (30%) 6 (67%) Anti-CTLA4 38 (81%) 8 (89%) BRAF inhibitor 7 (15%) 4 (44%) PRAME status (IHC) Positive3 42 (89%) 9
(100%) H-score4 – median 215 155 Patients were heavily pre-treated All received prior checkpoint inhibitors (CPI) Median 2 prior anti-PD1 regimens 81% prior ipilimumab – nearly all in combination with nivolumab 38% had another IO,
in addition to anti-PD1, anti-CTLA4 Pembro combo pts. more heavily pre-treated Higher percentage with prior BRAFi and primary resistance to anti-PD1 PRAME expression was high (median H score 215 in monotherapy)4
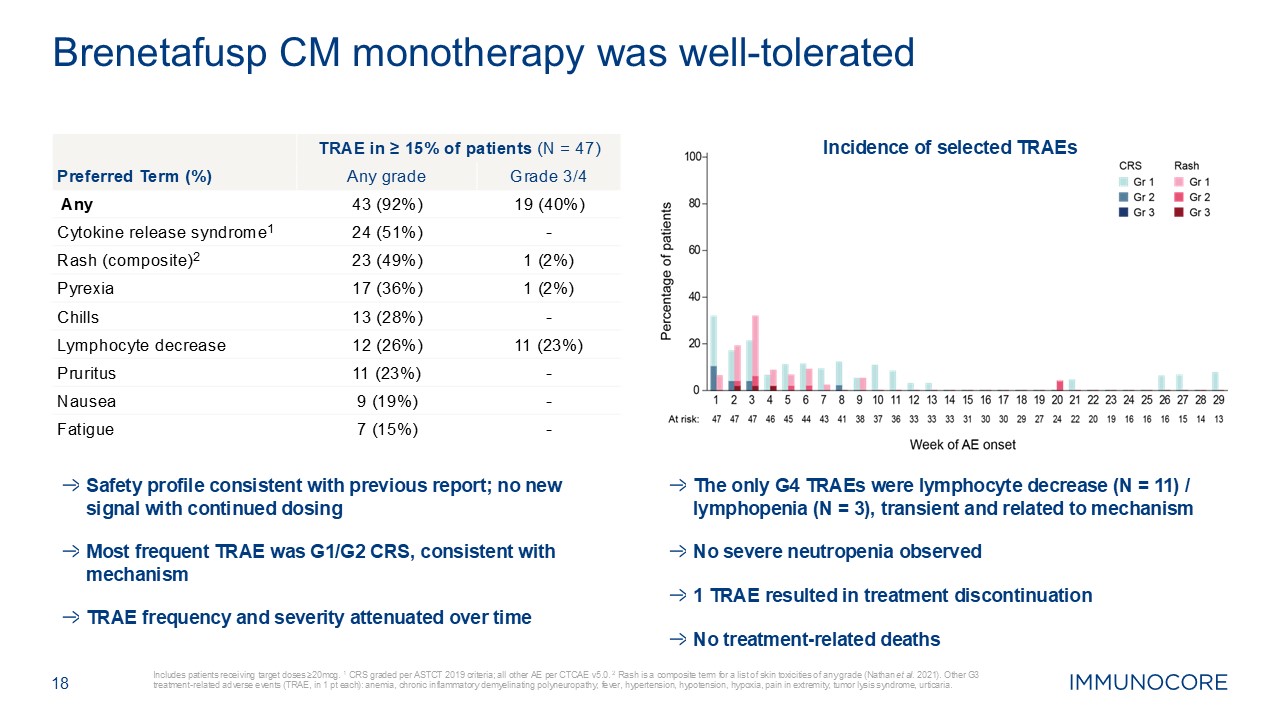
18 Includes patients receiving target doses ≥20mcg. 1 CRS graded per ASTCT
2019 criteria; all other AE per CTCAE v5.0. 2 Rash is a composite term for a list of skin toxicities of any grade (Nathan et al. 2021). Other G3 treatment-related adverse events (TRAE, in 1 pt each): anemia, chronic inflammatory
demyelinating polyneuropathy, fever, hypertension, hypotension, hypoxia, pain in extremity, tumor lysis syndrome, urticaria. Brenetafusp CM monotherapy was well-tolerated Incidence of selected TRAEs Safety profile consistent with
previous report; no new signal with continued dosing Most frequent TRAE was G1/G2 CRS, consistent with mechanism TRAE frequency and severity attenuated over time The only G4 TRAEs were lymphocyte decrease (N = 11) / lymphopenia (N = 3),
transient and related to mechanism No severe neutropenia observed 1 TRAE resulted in treatment discontinuation No treatment-related deaths TRAE in ≥ 15% of patients (N = 47) Preferred Term (%) Any grade Grade 3/4 Any 43 (92%) 19
(40%) Cytokine release syndrome1 24 (51%) - Rash (composite)2 23 (49%) 1 (2%) Pyrexia 17 (36%) 1 (2%) Chills 13 (28%) - Lymphocyte decrease 12 (26%) 11 (23%) Pruritus 11 (23%) - Nausea 9 (19%) - Fatigue 7 (15%) -
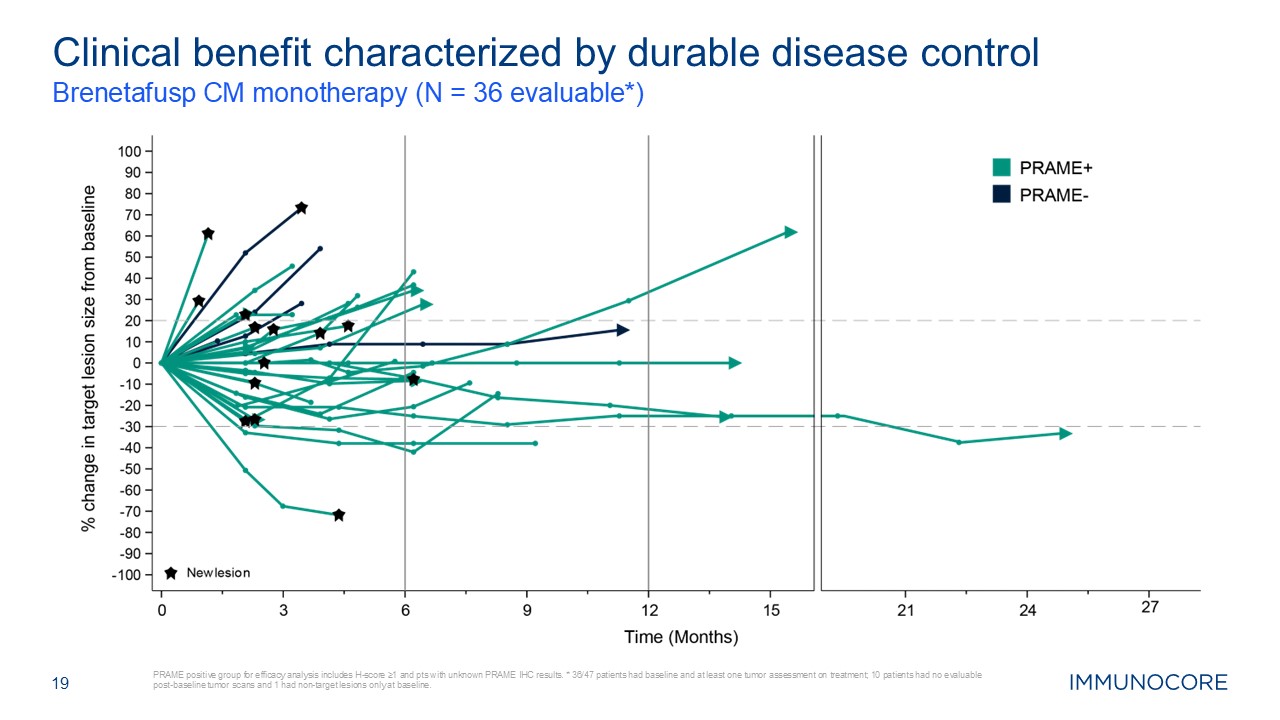
19 Brenetafusp CM monotherapy (N = 36 evaluable*) PRAME positive group for
efficacy analysis includes H-score ≥1 and pts with unknown PRAME IHC results. * 36/47 patients had baseline and at least one tumor assessment on treatment; 10 patients had no evaluable post-baseline tumor scans and 1 had non-target lesions
only at baseline. Clinical benefit characterized by durable disease control
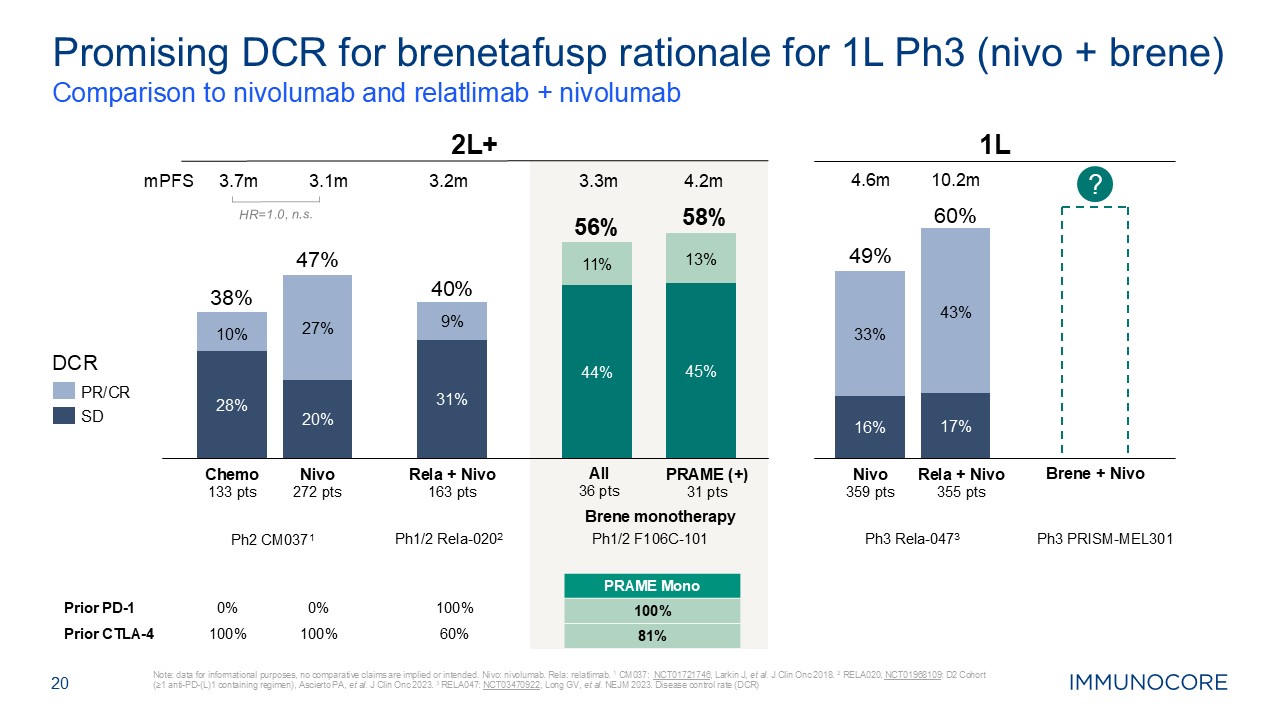
20 Comparison to nivolumab and relatlimab + nivolumab Note: data for
informational purposes, no comparative claims are implied or intended. Nivo: nivolumab. Rela: relatlimab. 1 CM037: NCT01721746, Larkin J, et al. J Clin Onc 2018. 2 RELA020, NCT01968109: D2 Cohort (≥1 anti-PD-(L)1 containing regimen),
Ascierto PA, et al. J Clin Onc 2023. 3 RELA047: NCT03470922, Long GV, et al. NEJM 2023. Disease control rate (DCR) Promising DCR for brenetafusp rationale for 1L Ph3 (nivo + brene) Prior PD-1 0% 0% 100% Prior
CTLA-4 100% 100% 60% Ph1/2 Rela-0202 Ph1/2 F106C-101 PRAME Mono 100% 81% All 36 pts PRAME (+) 31 pts 2L+ PR/CR SD DCR Nivo 272 pts Rela + Nivo 163
pts 8% 28% 27% 20% 31% 9% 38% 47% 40% 11% 44% 13% 45% 56% 58% Chemo 133 pts Ph2 CM0371 27% 20% 9% 31% 11% 44% 13% 45% HR=1.0, n.s. mPFS 3.7m 3.1m 3.2m 3.3m 4.2m 1L Rela + Nivo 355 pts 49% 60% Nivo 359
pts Ph3 Rela-0473 Ph3 PRISM-MEL301 ? Brene + Nivo 33% 16% 43% 17% 4.6m 10.2m Brene monotherapy 10% 28%
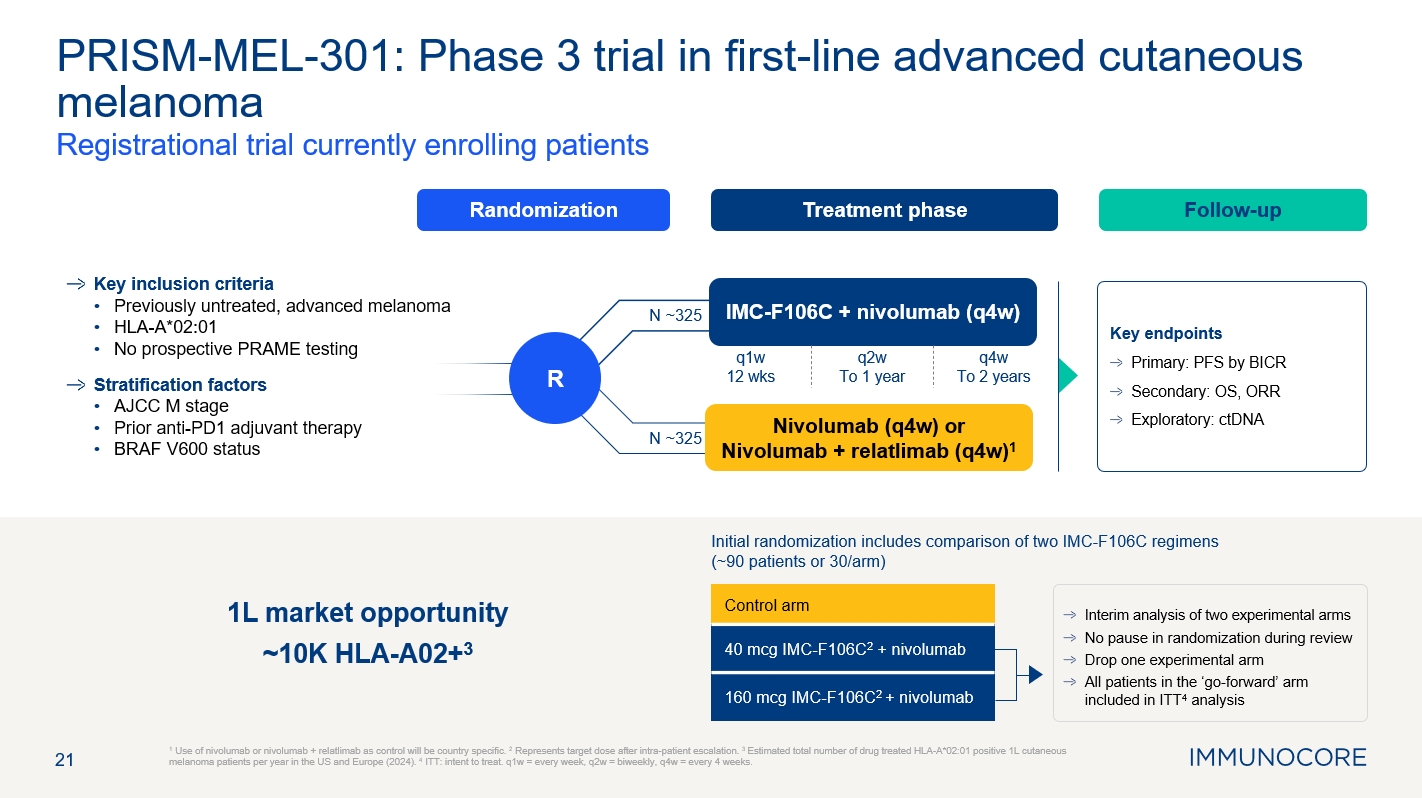
21 1 Use of nivolumab or nivolumab + relatlimab as control will be country
specific. 2 Represents target dose after intra-patient escalation. 3 Estimated total number of drug treated HLA-A*02:01 positive 1L cutaneous melanoma patients per year in the US and Europe (2024). 4 ITT: intent to treat. q1w = every week,
q2w = biweekly, q4w = every 4 weeks. PRISM-MEL-301: Phase 3 trial in first-line advanced cutaneous melanoma Registrational trial currently enrolling patients Treatment phase Follow-up Randomization R Key inclusion
criteria Previously untreated, advanced melanoma HLA-A*02:01 No prospective PRAME testing Stratification factors AJCC M stage Prior anti-PD1 adjuvant therapy BRAF V600 status Key endpoints Primary: PFS by BICR Secondary: OS,
ORR Exploratory: ctDNA IMC-F106C + nivolumab (q4w) Nivolumab (q4w) or Nivolumab + relatlimab (q4w)1 N ~325 N ~325 q1w 12 wks q2w To 1 year q4w To 2 years Control arm 40 mcg IMC-F106C2 + nivolumab 160 mcg IMC-F106C2 +
nivolumab Interim analysis of two experimental arms No pause in randomization during review Drop one experimental arm All patients in the ‘go-forward’ arm included in ITT4 analysis Initial randomization includes comparison of two
IMC-F106C regimens (~90 patients or 30/arm) 1L market opportunity ~10K PRAME+, HLA-A02+3

Brenetafusp in ovarian 22
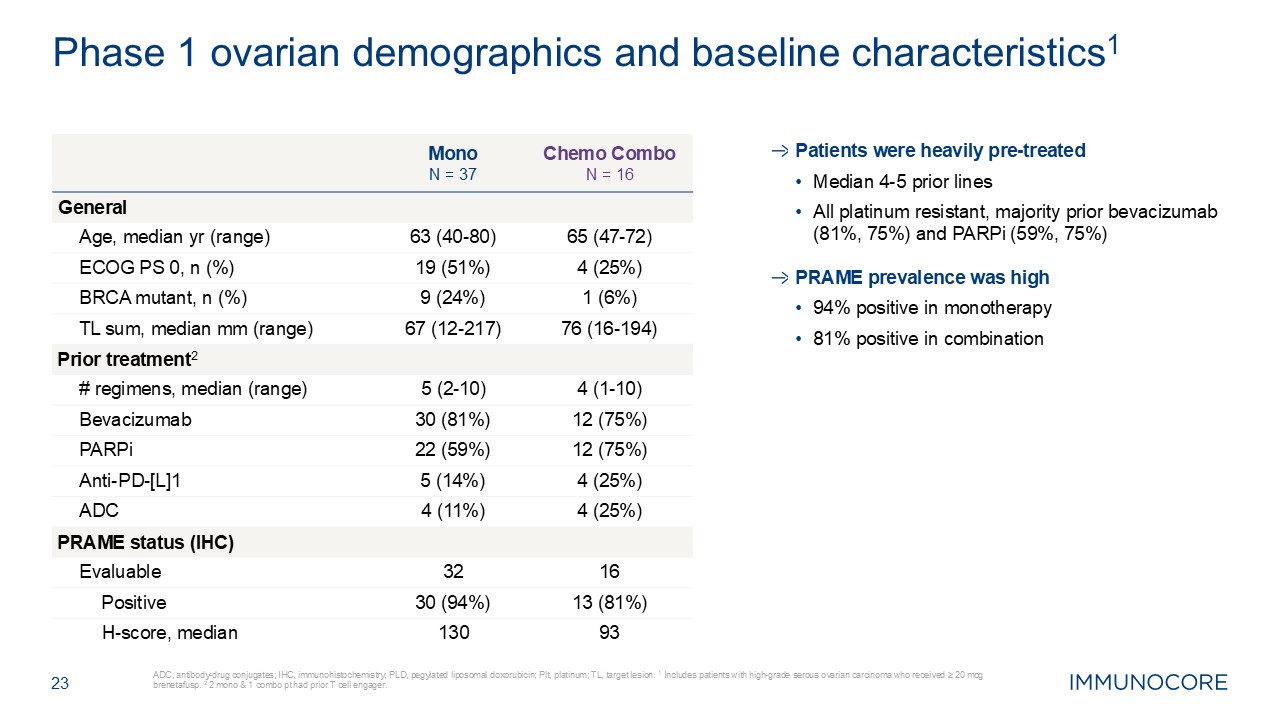
23 ADC, antibody-drug conjugates; IHC, immunohistochemistry; PLD, pegylated
liposomal doxorubicin; Plt, platinum; TL, target lesion. 1 Includes patients with high-grade serous ovarian carcinoma who received ≥ 20 mcg brenetafusp. 2 2 mono & 1 combo pt had prior T cell engager. Phase 1 ovarian demographics and
baseline characteristics1 Mono N = 37 Chemo Combo N = 16 General Age, median yr (range) 63 (40-80) 65 (47-72) ECOG PS 0, n (%) 19 (51%) 4 (25%) BRCA mutant, n (%) 9 (24%) 1 (6%) TL sum, median mm (range) 67 (12-217) 76
(16-194) Prior treatment2 # regimens, median (range) 5 (2-10) 4 (1-10) Bevacizumab 30 (81%) 12 (75%) PARPi 22 (59%) 12 (75%) Anti-PD-[L]1 5 (14%) 4 (25%) ADC 4 (11%) 4 (25%) PRAME status
(IHC) Evaluable 32 16 Positive 30 (94%) 13 (81%) H-score, median 130 93 Patients were heavily pre-treated Median 4-5 prior lines All platinum resistant, majority prior bevacizumab (81%, 75%) and PARPi (59%, 75%) PRAME
prevalence was high 94% positive in monotherapy 81% positive in combination
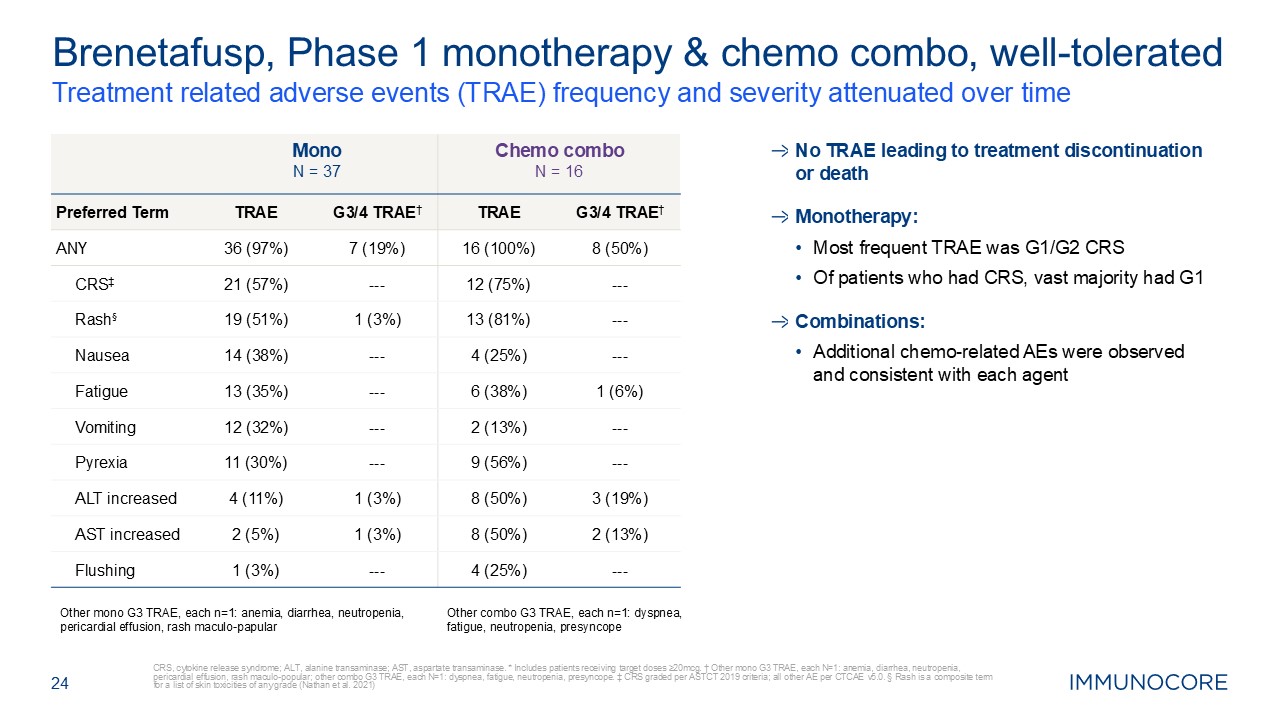
24 Treatment related adverse events (TRAE) frequency and severity attenuated
over time CRS, cytokine release syndrome; ALT, alanine transaminase; AST, aspartate transaminase. * Includes patients receiving target doses ≥20mcg. † Other mono G3 TRAE, each N=1: anemia, diarrhea, neutropenia, pericardial effusion, rash
maculo-popular; other combo G3 TRAE, each N=1: dyspnea, fatigue, neutropenia, presyncope. ‡ CRS graded per ASTCT 2019 criteria; all other AE per CTCAE v5.0. § Rash is a composite term for a list of skin toxicities of any grade (Nathan et
al. 2021) Brenetafusp, Phase 1 monotherapy & chemo combo, well-tolerated Mono N = 37 Chemo combo N = 16 Preferred Term TRAE G3/4 TRAE† TRAE G3/4 TRAE† ANY 36 (97%) 7 (19%) 16 (100%) 8 (50%) CRS‡ 21 (57%) --- 12
(75%) --- Rash§ 19 (51%) 1 (3%) 13 (81%) --- Nausea 14 (38%) --- 4 (25%) --- Fatigue 13 (35%) --- 6 (38%) 1 (6%) Vomiting 12 (32%) --- 2 (13%) --- Pyrexia 11 (30%) --- 9 (56%) --- ALT increased 4 (11%) 1 (3%) 8
(50%) 3 (19%) AST increased 2 (5%) 1 (3%) 8 (50%) 2 (13%) Flushing 1 (3%) --- 4 (25%) --- Other mono G3 TRAE, each n=1: anemia, diarrhea, neutropenia, pericardial effusion, rash maculo-papular Other combo G3 TRAE, each n=1:
dyspnea, fatigue, neutropenia, presyncope No TRAE leading to treatment discontinuation or death Monotherapy: Most frequent TRAE was G1/G2 CRS Of patients who had CRS, vast majority had G1 Combinations: Additional chemo-related AEs
were observed and consistent with each agent
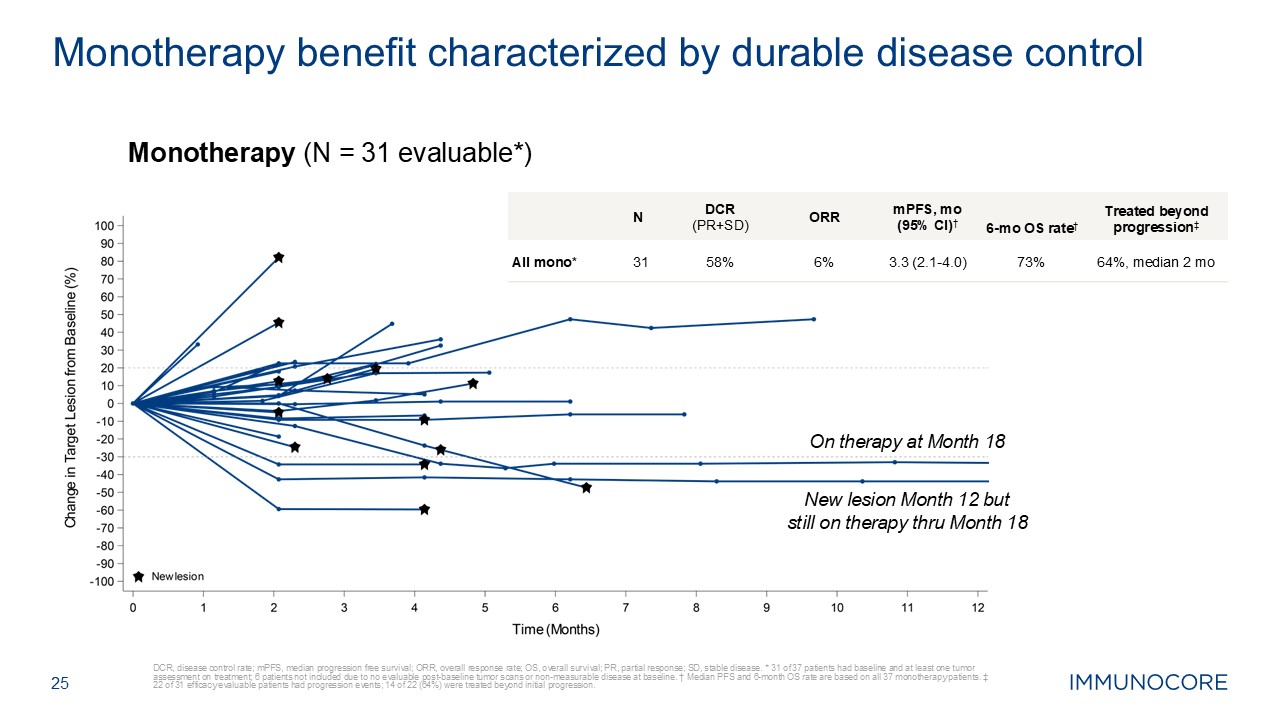
25 DCR, disease control rate; mPFS, median progression free survival; ORR,
overall response rate; OS, overall survival; PR, partial response; SD, stable disease. * 31 of 37 patients had baseline and at least one tumor assessment on treatment; 6 patients not included due to no evaluable post-baseline tumor scans or
non-measurable disease at baseline. † Median PFS and 6-month OS rate are based on all 37 monotherapy patients. ‡ 22 of 31 efficacy evaluable patients had progression events; 14 of 22 (64%) were treated beyond initial
progression. Monotherapy benefit characterized by durable disease control N DCR (PR+SD) ORR mPFS, mo (95% CI)† 6-mo OS rate† Treated beyond progression‡ All mono* 31 58% 6% 3.3 (2.1-4.0) 73% 64%, median 2 mo Monotherapy
(N = 31 evaluable*) On therapy at Month 18 New lesion Month 12 but still on therapy thru Month 18
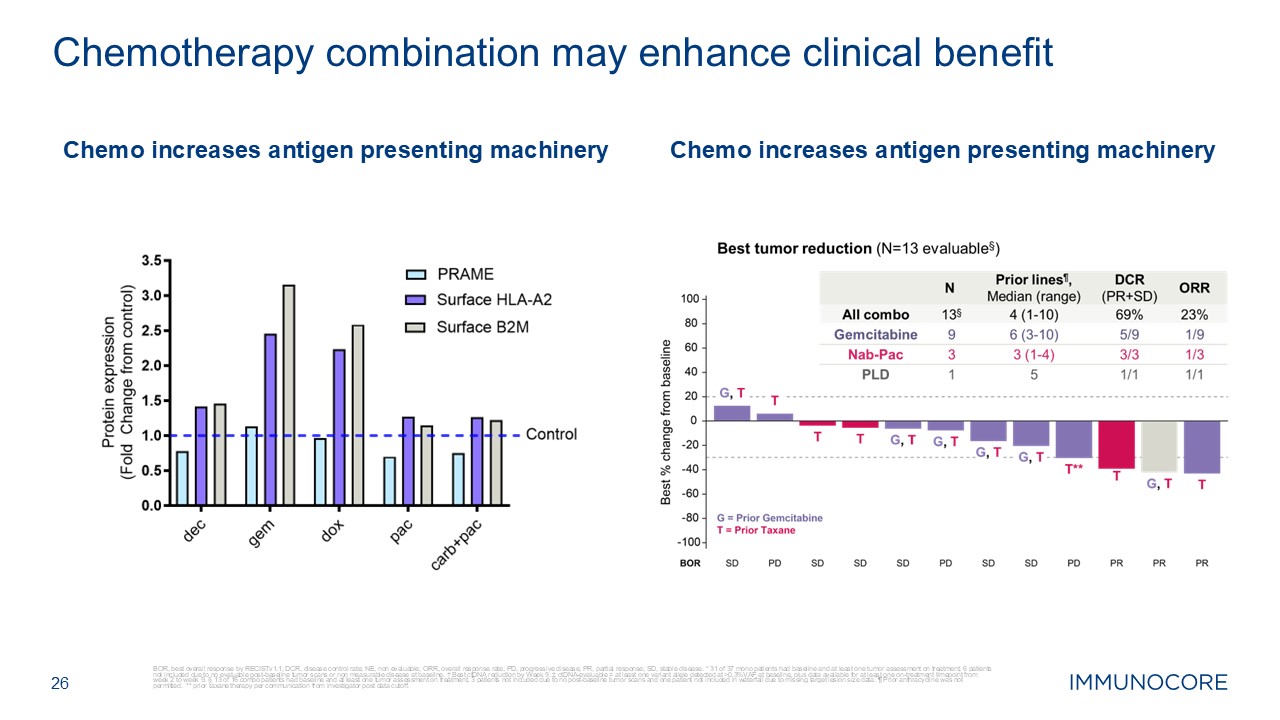
BOR, best overall response by RECISTv1.1; DCR, disease control rate; NE, non
evaluable; ORR, overall response rate; PD, progressive disease; PR, partial response; SD, stable disease. * 31 of 37 mono patients had baseline and at least one tumor assessment on treatment; 6 patients not included due to no evaluable
post-baseline tumor scans or non measurable disease at baseline. † Best ctDNA reduction by Week 9. ‡ ctDNA-evaluable = at least one variant allele detected at >0.3%VAF at baseline, plus data available for at least one on-treatment
timepoint from week 2 to week 9. § 13 of 16 combo patients had baseline and at least one tumor assessment on treatment; 3 patients not included due to no post-baseline tumor scans and one patient not included in waterfall due to missing
target lesion size data. ¶ Prior anthracycline was not permitted. ** prior taxane therapy per communication from investigator post data cutoff. 26 Chemotherapy combination may enhance clinical benefit Chemo increases antigen presenting
machinery Chemo increases antigen presenting machinery
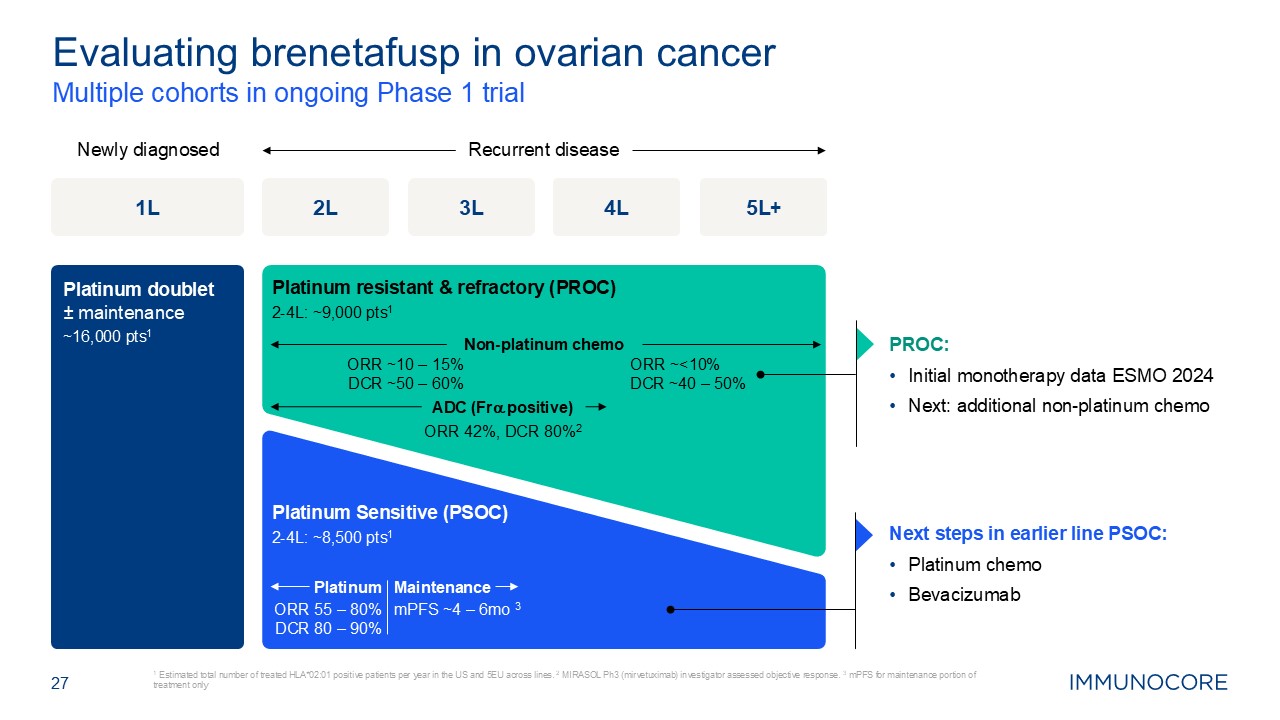
27 Multiple cohorts in ongoing Phase 1 trial 1 Estimated total number of
treated HLA*02:01 positive patients per year in the US and 5EU across lines. 2 MIRASOL Ph3 (mirvetuximab) investigator assessed objective response. 3 mPFS for maintenance portion of treatment only Evaluating brenetafusp in ovarian
cancer 1L 5L+ Recurrent disease Newly diagnosed Platinum doublet± maintenance ~16,000 pts1 2L 3L 4L PROC: Initial monotherapy data ESMO 2024 Next: additional non-platinum chemo Next steps in earlier line PSOC: Platinum chemo
Bevacizumab ORR 55 – 80% DCR 80 – 90% Maintenance ORR ~10 – 15% DCR ~50 – 60% Non-platinum chemo ORR ~<10% DCR ~40 – 50% Platinum mPFS ~4 – 6mo 3 ADC (Fra positive) ORR 42%, DCR 80%2 Platinum Sensitive (PSOC) 2-4L:
~8,500 pts1 Platinum resistant & refractory (PROC) 2-4L: ~9,000 pts1
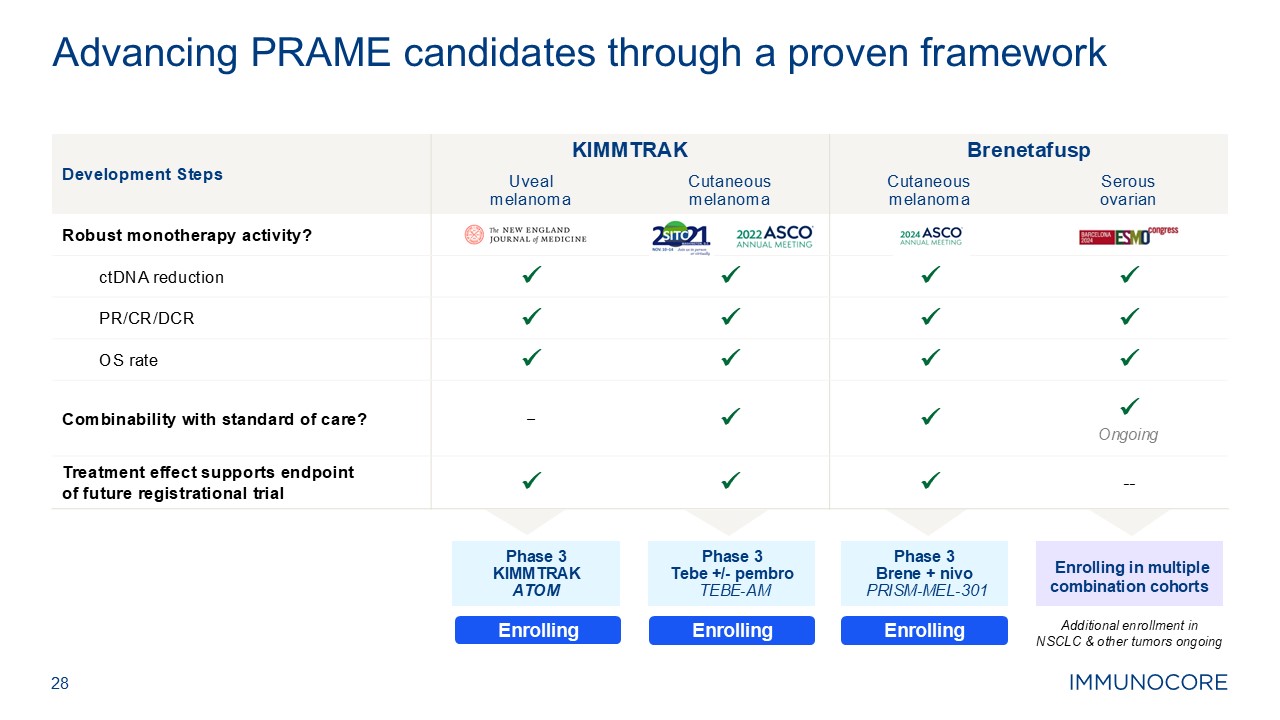
28 Advancing PRAME candidates through a proven framework Development
Steps KIMMTRAK Brenetafusp Uveal melanoma Cutaneous melanoma Cutaneous melanoma Serous ovarian Robust monotherapy activity? ctDNA reduction PR/CR/DCR OS rate Combinability with standard of
care? – Ongoing Treatment effect supports endpoint of future registrational trial -- Enrolling in multiple combination cohorts Phase 3 KIMMTRAK ATOM Phase 3 Tebe +/- pembro TEBE-AM Enrolling Phase 3
Brene + nivo PRISM-MEL-301 Enrolling Enrolling PRAME franchise expansion opportunities for HLE and A24 programs (IND/Ph1) Additional enrollment in NSCLC & other tumors ongoing
T Cell Fitness (TCF) 29
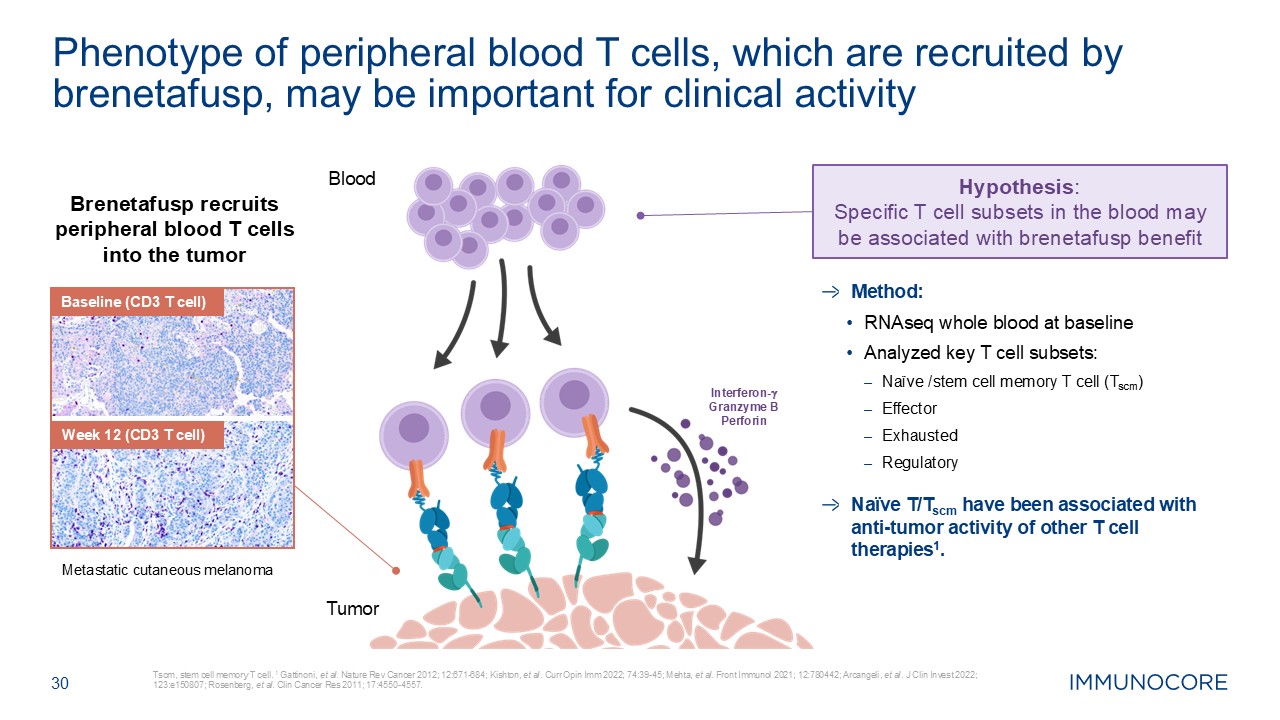
30 Tscm, stem cell memory T cell. 1 Gattinoni, et al. Nature Rev Cancer 2012;
12:671-684; Kishton, et al. Curr Opin Imm 2022; 74:39-45; Mehta, et al. Front Immunol 2021; 12:780442; Arcangeli, et al. J Clin Invest 2022; 123:e150807; Rosenberg, et al. Clin Cancer Res 2011; 17:4550-4557. Phenotype of peripheral blood T
cells, which are recruited by brenetafusp, may be important for clinical activity Brenetafusp recruits peripheral blood T cells into the tumor Metastatic cutaneous melanoma Baseline (CD3 T cell) Week 12 (CD3 T cell) Hypothesis:
Specific T cell subsets in the blood may be associated with brenetafusp benefit Interferon-g Granzyme B Perforin Blood Tumor Method: RNAseq whole blood at baseline Analyzed key T cell subsets: Naïve /stem cell memory T cell
(Tscm) Effector Exhausted Regulatory Naïve T/Tscm have been associated with anti-tumor activity of other T cell therapies1.
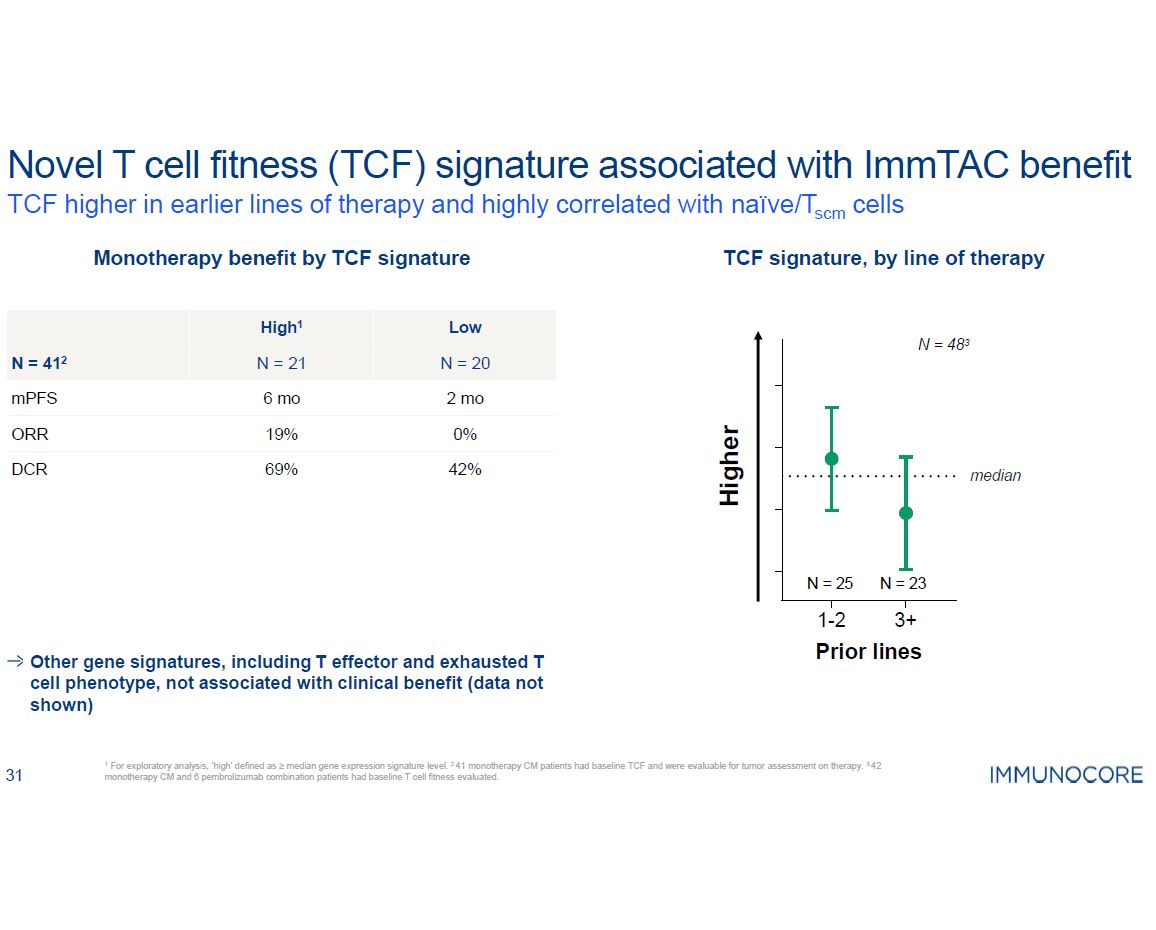
31 TCF higher in earlier lines of therapy and highly correlated with
naïve/Tscm cells a TCF association with overall survival (OS) in multivariate analysis adjusted for known mUM prognostic variables: LDH, ALP, lesion diameter >3cm, ECOG CONFIDENTIAL - FOR INTERNAL USE TCF in blood associated with OS
and higher ORR OS, by TCF signature in uveal melanoma Higher ORR in high TCF group But not high enough for accelerated approval TCF Tebe mUM PRAME mUM PRAME CM PRAME
Ovarian High 9% 27% 19% 13% Low 2% 0 0 0% Unstratified 5% 14% 10% 7%
Novel ImmTAC candidate for GI cancers from our discovery engine 32
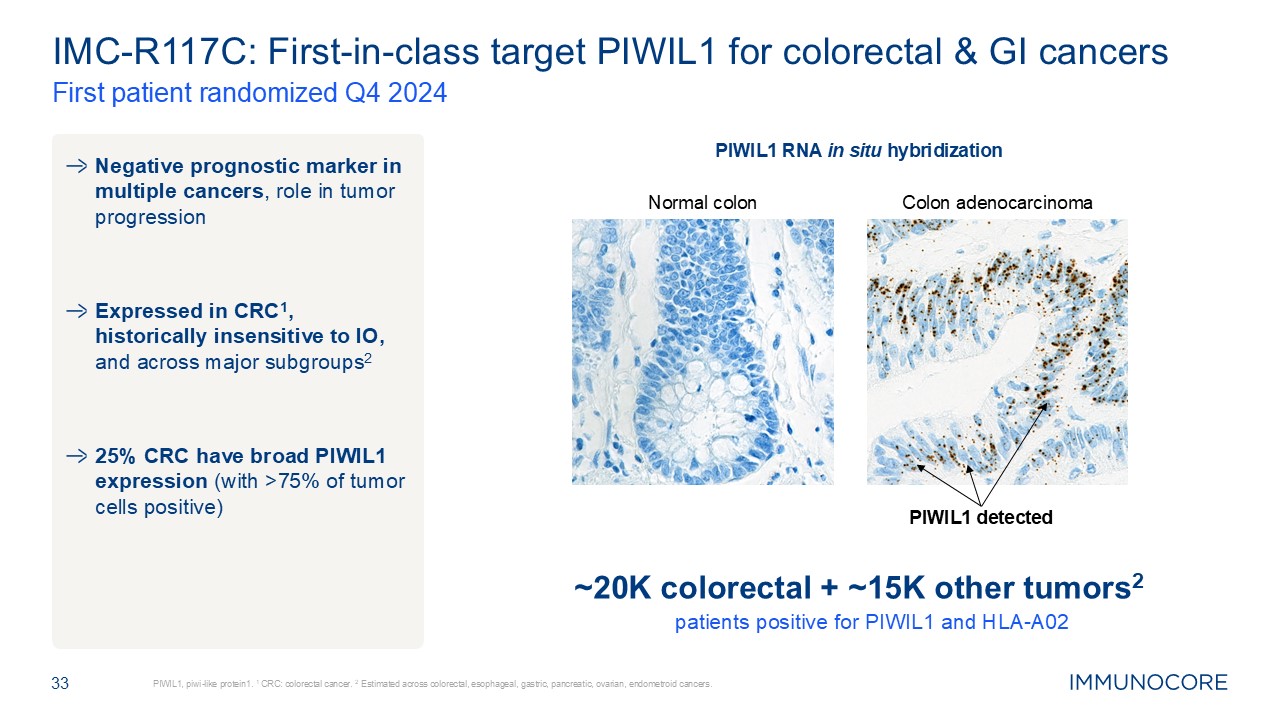
33 PIWIL1, piwi-like protein1. 1 CRC: colorectal cancer. 2 Estimated across
colorectal, esophageal, gastric, pancreatic, ovarian, endometroid cancers. First patient randomized Q4 2024 IMC-R117C: First-in-class target PIWIL1 for colorectal & GI cancers Negative prognostic marker in multiple cancers, role in
tumor progression Expressed in CRC1, historically insensitive to IO, and across major subgroups2 25% CRC have broad PIWIL1 expression (with >75% of tumor cells positive) Colon adenocarcinoma Normal colon PIWIL1 detected PIWIL1 RNA
in situ hybridization ~20K colorectal + ~15K other tumors2 patients positive for PIWIL1 and HLA-A02
Pursuing a functional cure in infectious diseases 34
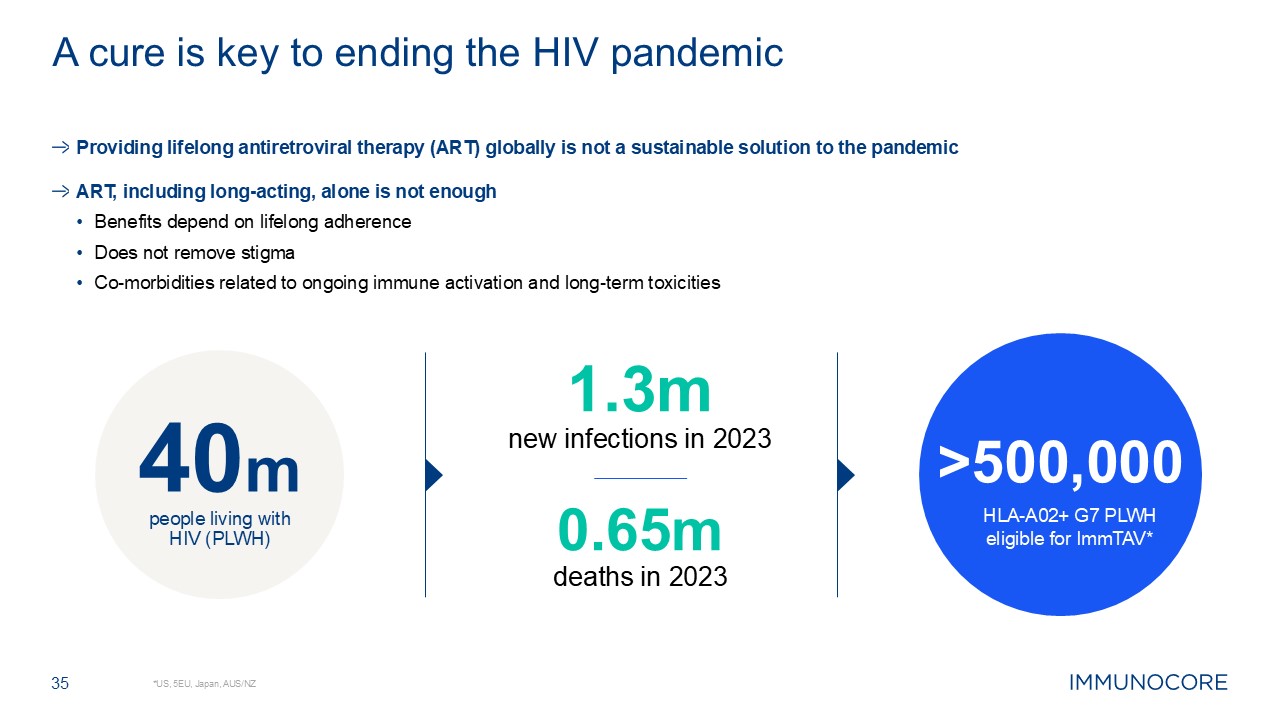
40m people living with HIV (PLWH) HLA-A02+ G7 PLWH eligible for
ImmTAV* >500,000 35 *US, 5EU, Japan, AUS/NZ A cure is key to ending the HIV pandemic Providing lifelong antiretroviral therapy (ART) globally is not a sustainable solution to the pandemic ART, including long-acting, alone is not
enough Benefits depend on lifelong adherence Does not remove stigma Co-morbidities related to ongoing immune activation and long-term toxicities 1.3m new infections in 2023 0.65m deaths in 2023
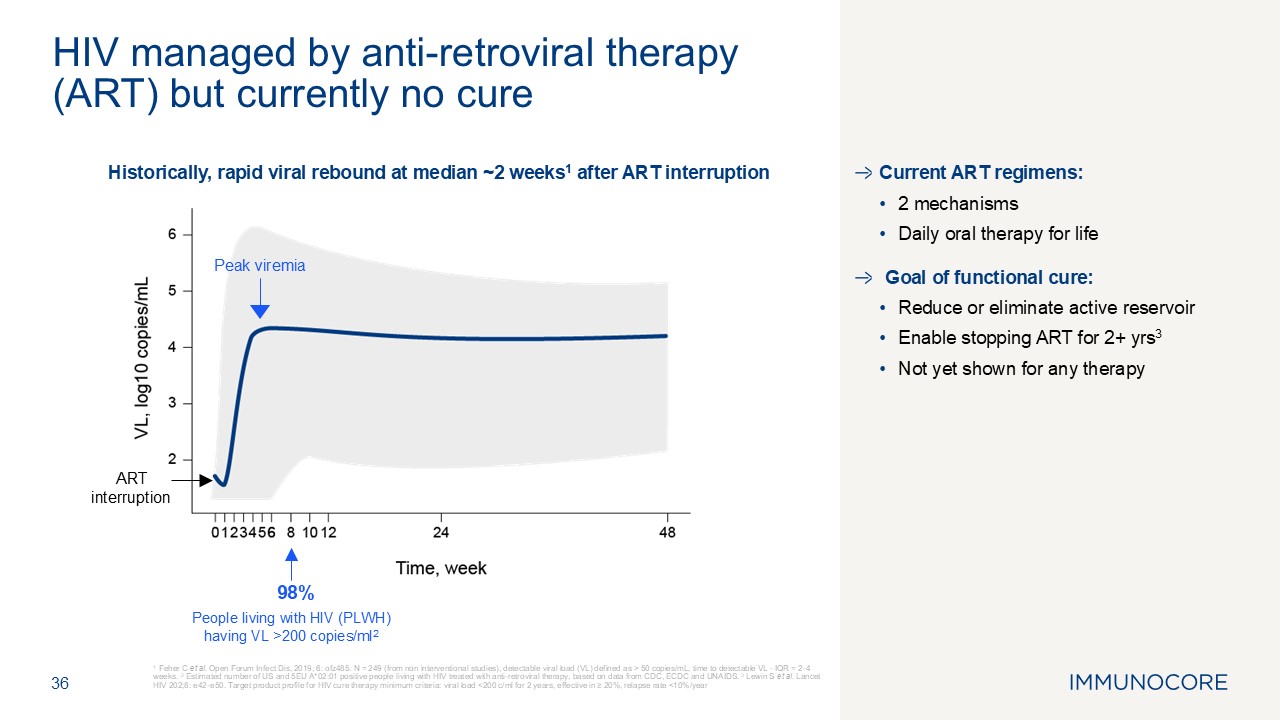
Historically, rapid viral rebound at median ~2 weeks1 after ART
interruption Current ART regimens: 2 mechanisms Daily oral therapy for life Goal of functional cure: Reduce or eliminate active reservoir Enable stopping ART for 2+ yrs3 Not yet shown for any therapy 36 1 Feher C et al. Open
Forum Infect Dis, 2019; 6: ofz485. N = 249 (from non interventional studies), detectable viral load (VL) defined as > 50 copies/mL, time to detectable VL - IQR = 2-4 weeks. 2 Estimated number of US and 5EU A*02:01 positive people living
with HIV treated with anti-retroviral therapy, based on data from CDC, ECDC and UNAIDS. 3 Lewin S et al. Lancet HIV 202;8: e42-e50. Target product profile for HIV cure therapy minimum criteria: viral load <200 c/ml for 2 years, effective
in ≥ 20%, relapse rate <10%/year HIV managed by anti-retroviral therapy (ART) but currently no cure 98% Peak viremia ART interruption People living with HIV (PLWH) having VL >200 copies/ml2
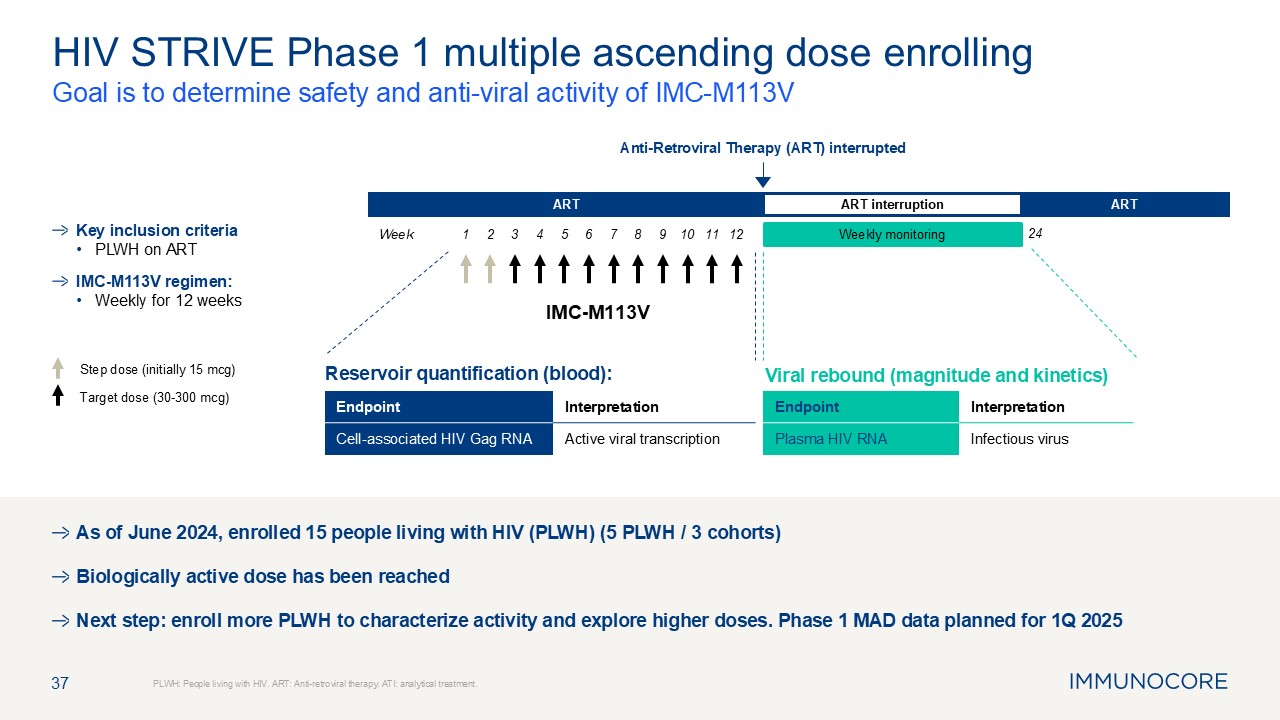
37 Goal is to determine safety and anti-viral activity of IMC-M113V PLWH:
People living with HIV. ART: Anti-retroviral therapy. ATI: analytical treatment. HIV STRIVE Phase 1 multiple ascending dose enrolling Key inclusion criteria PLWH on ART IMC-M113V regimen: Weekly for 12 weeks Step dose (initially 15
mcg) Target dose (30-300 mcg) Viral rebound (magnitude and kinetics) IMC-M113V Week ART Follow-up ART ART interruption Anti-Retroviral Therapy (ART) interrupted Weekly monitoring Reservoir quantification
(blood): 1 2 3 4 5 6 7 8 9 10 11 12 24 Endpoint Interpretation Cell-associated HIV Gag RNA Active viral transcription Endpoint Interpretation Plasma HIV RNA Infectious virus As of June 2024, enrolled 15 people living
with HIV (PLWH) (5 PLWH / 3 cohorts) Biologically active dose has been reached Next step: enroll more PLWH to characterize activity and explore higher doses. Phase 1 MAD data planned for 1Q 2025

Pioneering tissue-specific immune downmodulation for treatment of autoimmune
diseases 38
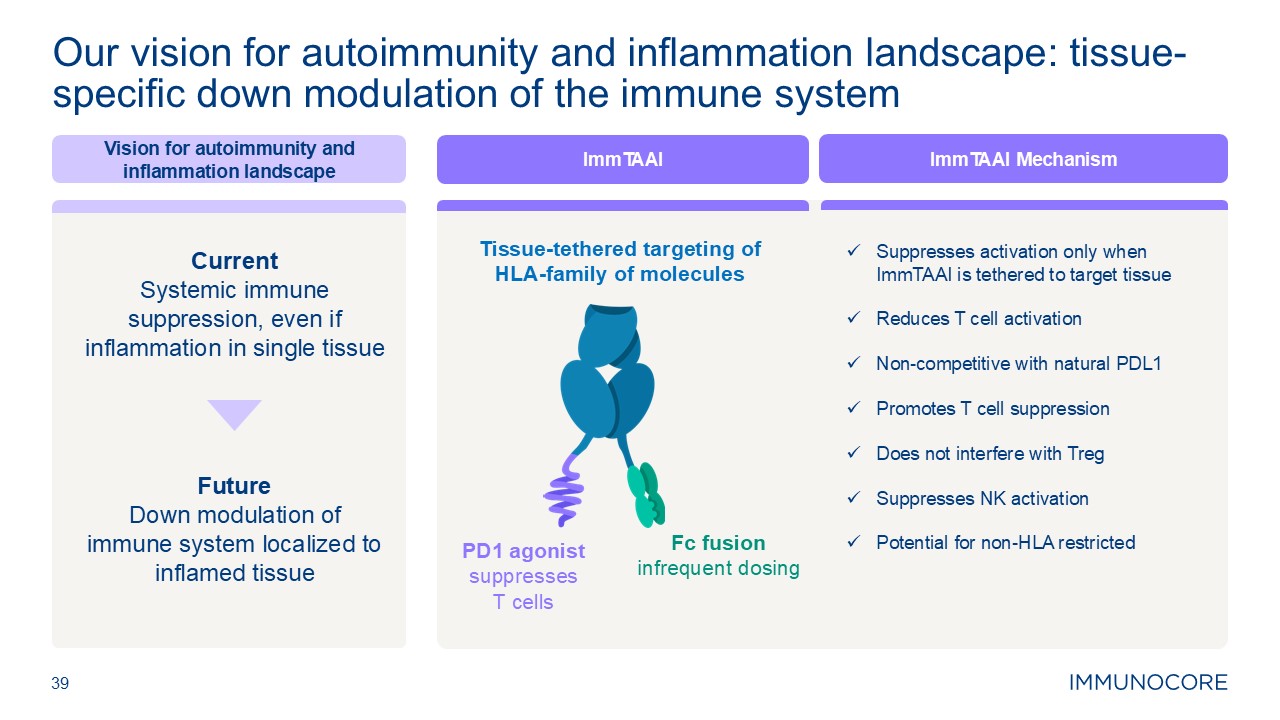
39 Our vision for autoimmunity and inflammation landscape: tissue-specific
down modulation of the immune system Vision for autoimmunity and inflammation landscape Current Systemic immune suppression, even if inflammation in single tissue Future Down modulation of immune system localized to inflamed
tissue Tissue-tethered targeting of HLA-family of molecules PD1 agonist suppresses T cells Fc fusion infrequent dosing ImmTAAI ImmTAAI Mechanism Suppresses activation only when ImmTAAI is tethered to target tissue Reduces T
cell activation Non-competitive with natural PDL1 Promotes T cell suppression Does not interfere with Treg Suppresses NK activation Potential for non-HLA restricted
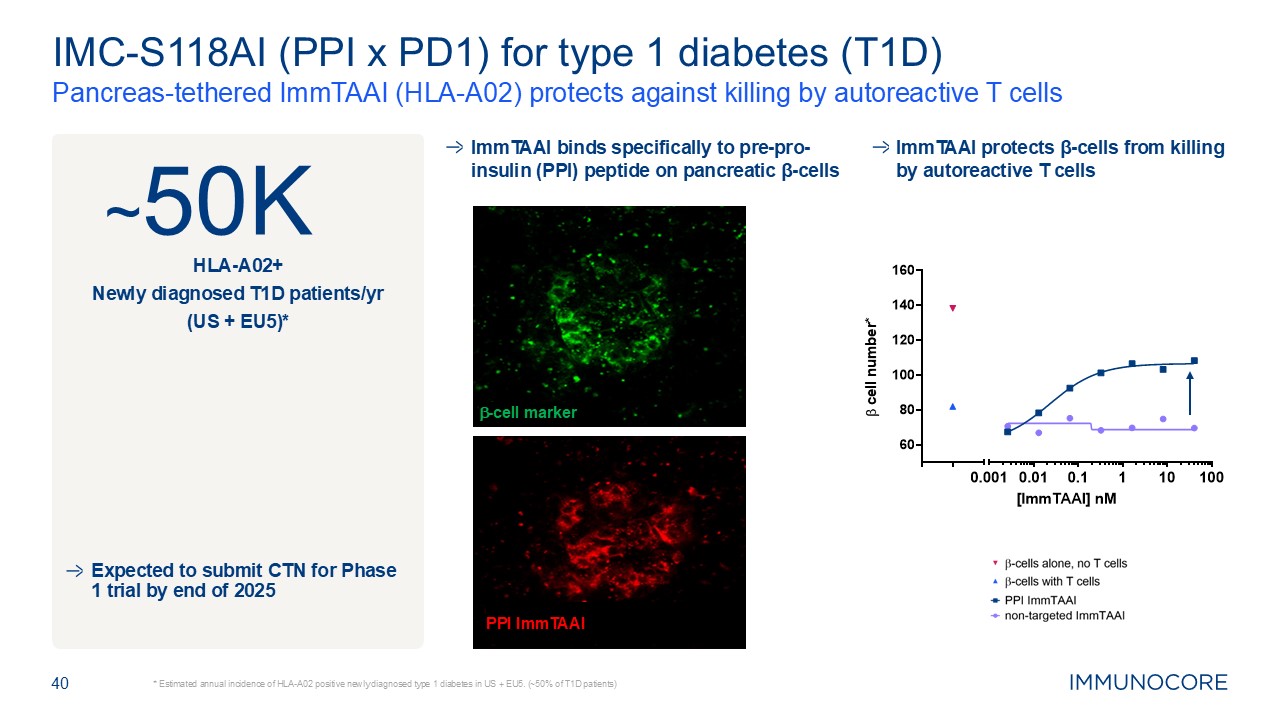
40 * Estimated annual incidence of HLA-A02 positive newly diagnosed type 1
diabetes in US + EU5. (~50% of T1D patients) Pancreas-tethered ImmTAAI (HLA-A02) protects against killing by autoreactive T cells IMC-S118AI (PPI x PD1) for type 1 diabetes (T1D) ~50K HLA-A02+ Newly diagnosed T1D patients/yr (US +
EU5)* Expected to submit CTN for Phase 1 trial by end of 2025 ImmTAAI protects β-cells from killing by autoreactive T cells b cell number* HLA-A02 restricted, ~50% of type 1 diabetes patients ImmTAAI binds specifically to
pre-pro-insulin (PPI) peptide on pancreatic β-cells b-cell marker PPI ImmTAAI
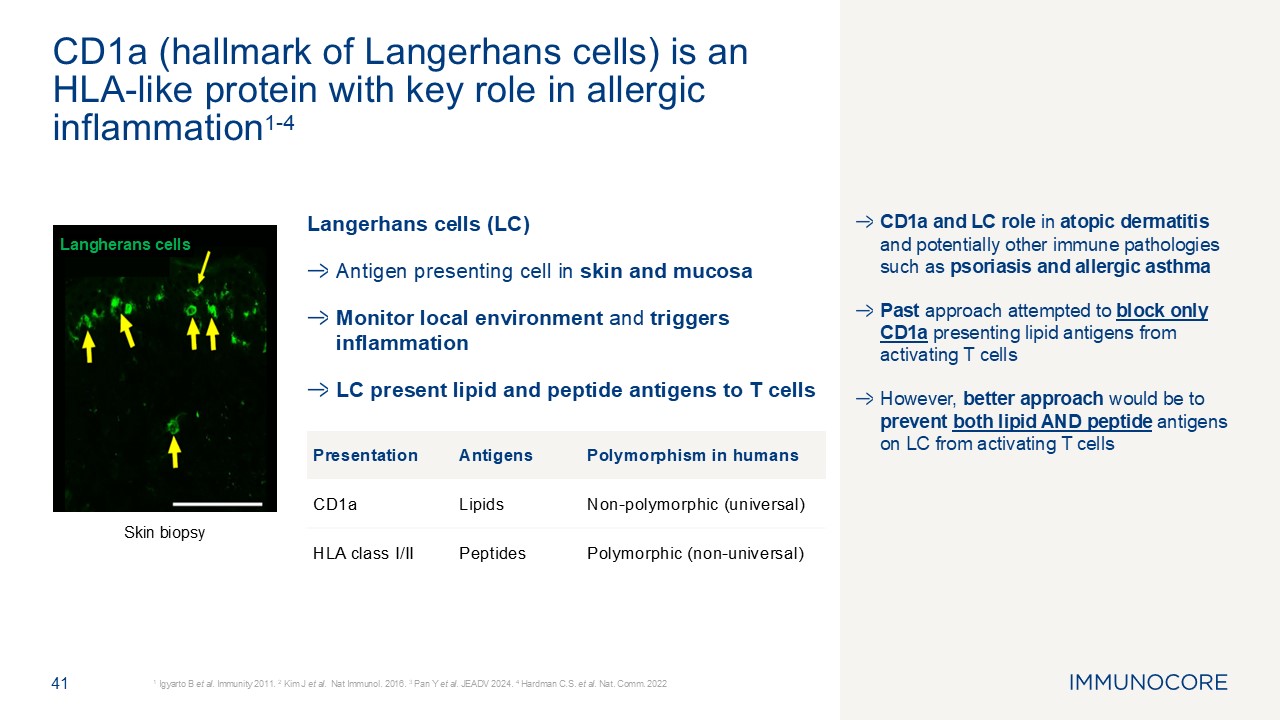
CD1a and LC role in atopic dermatitis and potentially other immune pathologies
such as psoriasis and allergic asthma Past approach attempted to block only CD1a presenting lipid antigens from activating T cells However, better approach would be to prevent both lipid AND peptide antigens on LC from activating T
cells 41 1 Igyarto B et al. Immunity 2011. 2 Kim J et al. Nat Immunol. 2016. 3 Pan Y et al. JEADV 2024. 4 Hardman C.S. et al. Nat. Comm. 2022 CD1a (hallmark of Langerhans cells) is an HLA-like protein with key role in allergic
inflammation1-4 Langherans cells Langerhans cells (LC) Antigen presenting cell in skin and mucosa Monitor local environment and triggers inflammation LC present lipid and peptide antigens to T cells Skin biopsy Presentation
Antigens Polymorphism in humans CD1a Lipids Non-polymorphic (universal) HLA class I/II Peptides Polymorphic (non-universal)
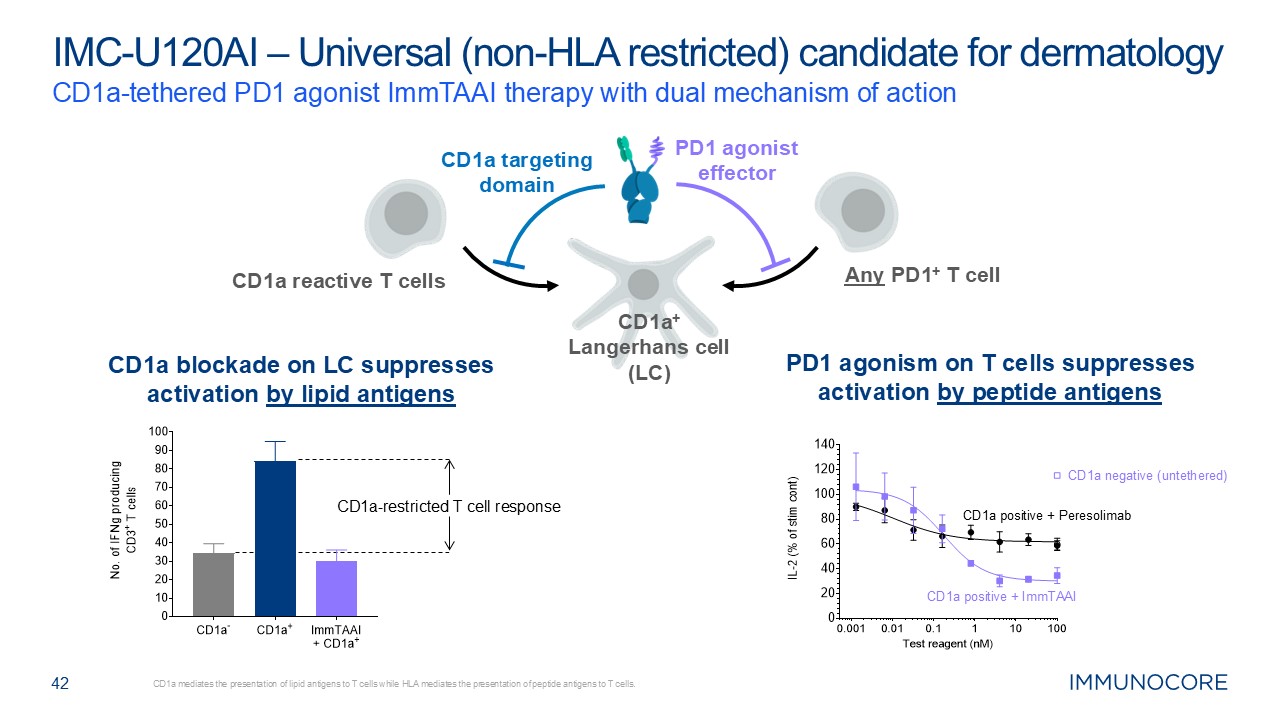
42 CD1a-tethered PD1 agonist ImmTAAI therapy with dual mechanism of
action CD1a mediates the presentation of lipid antigens to T cells while HLA mediates the presentation of peptide antigens to T cells. IMC-U120AI – Universal (non-HLA restricted) candidate for dermatology CD1a+ Langerhans cell (LC) CD1a
targeting domain PD1 agonist effector CD1a blockade on LC suppresses activation by lipid antigens PD1 agonism on T cells suppresses activation by peptide antigens CD1a-restricted T cell response CD1a positive + ImmTAAI CD1a negative
(untethered) CD1a positive + Peresolimab CD1a reactive T cells Any PD1+ T cell
Leading TCR pipeline 43
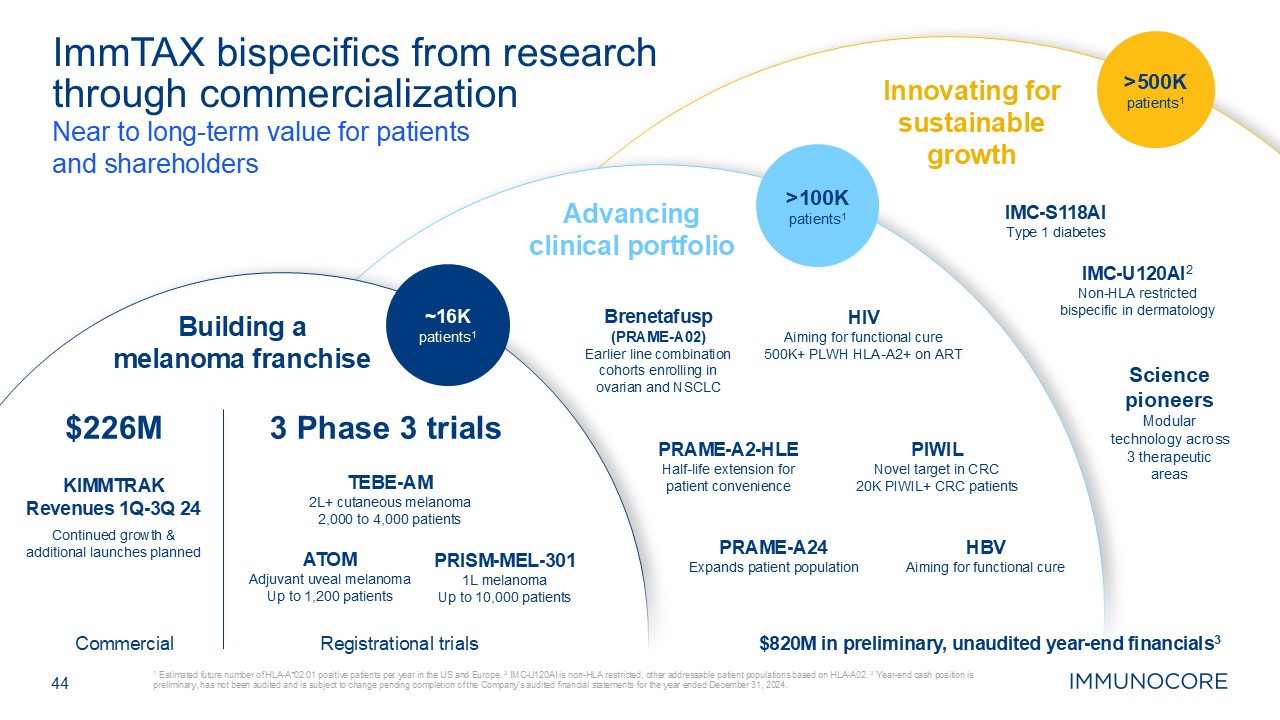
44 1 Estimated future number of HLA-A*02:01 positive patients per year in the
US and Europe. 2 IMC-U120AI is non-HLA restricted, other addressable patient populations based on HLA-A02. 3 Year-end cash position is preliminary, has not been audited and is subject to change pending completion of the Company’s audited
financial statements for the year ended December 31, 2024. ImmTAX bispecifics from research through commercialization Near to long-term value for patients and shareholders Innovating for sustainable growth Advancing clinical
portfolio Building a melanoma franchise Science pioneers Modular technology across 3 therapeutic areas PRAME-A2-HLE Half-life extension for patient convenience PIWIL Novel target in CRC 20K PIWIL+ CRC patients IMC-S118AI Type 1
diabetes IMC-U120AI2 Non-HLA restricted bispecific in dermatology PRAME-A24 Expands patient population Brenetafusp (PRAME-A02) Earlier line combination cohorts enrolling in ovarian and NSCLC HIV Aiming for functional cure 500K+
PLWH HLA-A2+ on ART Commercial $226M ATOM Adjuvant uveal melanoma Up to 1,200 patients TEBE-AM 2L+ cutaneous melanoma 2,000 to 4,000 patients PRISM-MEL-301 1L melanoma Up to 10,000 patients 3 Phase 3 trials Registrational
trials KIMMTRAK Revenues 1Q-3Q 24 Continued growth & additional launches planned ~16K patients1 >500K patients1 >100Kpatients1 HBV Aiming for functional cure $820M in preliminary, unaudited year-end financials3
Thank you 45